$26 million awarded to Washington University for leukemia research
A $26 million grant has been awarded to study the genetic underpinnings of leukemia and help improve treatment and outcomes for patients
The National Cancer Institute, part of the National Institutes of Health (NIH), has awarded two major grants totaling $26 million to leukemia researchers and physicians at the Alvin J. Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine.
The funding helps establish the School of Medicine as a premier center for innovative leukemia research, with a bench-to-beside approach that has the potential to lead to novel therapies that improve survival and reduce treatment-related adverse side effects.
Identifying leukemia’s genetic signatures
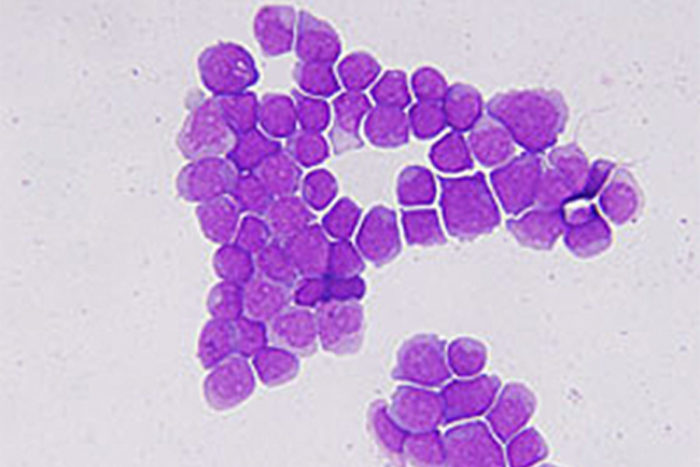
The first award is a five-year, $14.3 million Program Project Grant (PPG) to study leukemia. The grant was initially funded at the School of Medicine in 2003 and has been renewed twice. With this new support, researchers working on the project are looking to identify all the genetic changes that contribute to acute myeloid leukemia, the most common type of acute leukemia in adults. This information may lead to the development of more personalized treatments for patients based on the genetic makeup of their leukemia cells.
The second award is a prestigious Specialized Program of Research Excellence (SPORE) grant in leukemia. The $11.3 million, five-year award seeks to advance research done at the medical school to bring potential new treatments into clinical trials.

“The awards recognize the tremendous scientific depth and breadth of our scientists and clinicians as well as their creativity and commitment to improving treatments for leukemia,” said Daniel Link, MD, the Alan A. and Edith L. Wolff Professor of Medicine and principal investigator of the SPORE grant. “Thanks to advances in genomics and molecular biology, we’re on the cusp of a new way of thinking about leukemia and its treatment. There’s a lot to be excited about.”
The two grants bring together several dozens of physician scientists and basic research scientists who will be involved in a broad portfolio of laboratory and clinical research projects.
The two grants are closely related. “The PPG focuses on basic research to generate ideas, concepts and technologies that can be evaluated in clinical trials via the SPORE grant,” said Timothy Ley, MD, the Lewis T. and Rosalind B. Apple Chair in Oncology and principal investigator of the Program Project Grant.
Improving treatments and outcomes
The SPORE grant supports four new projects that may improve treatments and outcomes for patients with acute leukemia. The projects involve
- using genomics, the study of patients’ genomes. to help predict their response to chemotherapy
- developing novel therapies for acute myeloid leukemia and acute lymphocytic leukemia
- testing a new approach to reduce potentially deadly complications that arise in a stem cell transplant (a procedure that replaces diseased stem cells with healthy cells in leukemia patients)
Clinical trials at the School of Medicine will evaluate these new treatments and therapeutic approaches. Their success would lead to larger clinical studies in cooperation with other institutions.

The Program Project Grant involves four laboratory-based projects that target acute myeloid leukemia. About 80 percent of patients with this subtype of leukemia die within five years, when chemotherapy fails to keep the cancer in remission and the disease returns.
The new research involves looking at the genetic rules that help determine whether a leukemia patient will relapse.
This work could lead to:
- the development of new ways to predict relapses
- a better understanding of why some patients develop leukemia after treatment for other cancers
- the potential to define inherited mutations, or genetic changes, that dramatically increase the risk of acute myeloid leukemia in some families.







