Zika virus helps destroy deadly brain cancer in mice
Virus-based therapy may unlock potential of immunotherapy for glioblastoma
 Getty Images
Getty ImagesZika virus can activate immune cells to destroy an aggressive brain cancer in mice, giving a powerful boost to an immunotherapy drug and sparking long-lasting immunological memory that can ward off tumor recurrence for at least 18 months, according to a study from researchers at Washington University School of Medicine in St. Louis.
The Zika virus that ravaged the Americas, leaving many babies with permanent brain damage, may have a silver lining. The virus can activate immune cells to destroy an aggressive brain cancer in mice, giving a powerful boost to an immunotherapy drug and sparking long-lasting immunological memory that can ward off tumor recurrence for at least 18 months, according to a study from researchers at Washington University School of Medicine in St. Louis.
The findings, available online in the journal JCI Insight, suggest Zika virus might be a key to unlocking the power of immunotherapy for glioblastoma, a lethal brain cancer that typically results in death within two years. Immunotherapy aims to turn the body’s own immune system into a weapon to eliminate cancer cells. The approach has proven effective for blood, skin and some other cancers, but it has so far shown limited benefit for glioblastoma patients.
“Glioblastoma is a difficult disease because it progresses so quickly, and we don’t have any interventions that ultimately alter its course,” said co-senior author Milan G. Chheda, MD, an assistant professor of medicine and of neurology. “We can treat the initial tumor, but recurrence is quick and inevitable. By using Zika virus, we’re revving up the immune system to respond to an otherwise ineffective immunotherapy. This also sets the stage to prevent recurrence, allowing us to overcome two major barriers to effective treatment.”
Glioblastoma is the most common and aggressive form of brain cancer. About 12,000 people are diagnosed each year in the U.S., and average survival time is only 14 months. In 2017, Chheda and co-senior author Michael S. Diamond, MD, PhD, the Herbert S. Gasser Professor of Medicine and a professor of molecular microbiology, and of pathology & immunology, showed that Zika virus kills brain cancer stem cells, the kind of cells most resistant to standard treatments.
To better understand how Zika virus works against brain cancer, Chheda, Diamond and colleagues — including co-first authors Sharmila Nair, PhD, an instructor in medicine, and Luciano Mazzoccoli, PhD, and Arijita Jash, PhD, both postdoctoral researchers in Chheda’s lab — transplanted brain cancer cells into the brains of mice. One week later, they injected Zika virus into the mice’s quickly growing tumors, or sterile saltwater for comparison.
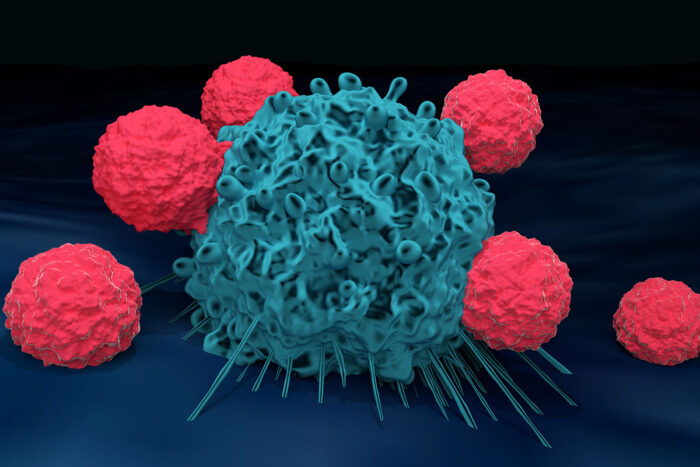
Zika virus treatment improved the animals’ chance of survival dramatically: to 63% from 10% for one cancer cell line, and to 37% from 0% for the other. Further analysis showed that the virus had attracted large numbers of immune cells of many kinds to the tumors, most importantly so-called cytotoxic T cells, a type of immune cell specialized for killing cancerous cells.
What’s more, Zika virus treatment induced lasting immunological memory. The researchers re-introduced the tumor into the other side of the mice’s brains a year and a half after the original tumor. All but one of the mice destroyed the new tumor within a few weeks.
Many tumors create suppressive environments around themselves that hinder an effective immune response. The suppression is created, in part, by so-called immune checkpoint molecules such as PD-1 that keep immune cells that kill cancer cells – called cytotoxic T cells – turned “off” and unable to attack. Immunotherapy drugs that target PD-1 have been used successfully to treat skin, blood, lung and other cancers.
But not glioblastoma. Along with keeping immune cells turned off, glioblastomas manage to keep most of them at bay. Activating immune cells is not enough to eradicate a tumor if there are only a handful of immune cells around, Chheda said. But, he continued, Zika virus’s ability to attract large numbers of immune cells to the tumor — combined with immunotherapy to free them from suppression — might tip the balance toward tumor destruction.
To find out, the researchers implanted cancer cells in mice’s brains and then treated the animals with Zika virus, an antibody that inhibits PD-1, both or neither. Zika virus treatment alone and PD-1 inhibition alone each increased survival to about 60% from about 30%. The combination brought the survival rate close to 90%.
The results are promising, but Zika virus is best known for causing brain damage in fetuses, so any therapy that involves putting the virus in people’s brains raises safety concerns. The researchers repeated key experiments with a weakened form of the virus and found the same promising cancer-fighting results, albeit not quite as pronounced. They are planning additional studies to evaluate the safety and efficacy of the weakened virus as a treatment for patients with glioblastoma.







