Zika diagnostic test granted market authorization by FDA
Test based on Washington University research can detect signs of Zika infection in serum
 Getty Images
Getty ImagesA test for signs of Zika infection has been granted market authorization by the Food and Drug Administration. The test is based in part on an antibody developed by researchers at Washington University School of Medicine in St. Louis.
Zika virus can cause babies to be born with devastating brain damage. But the signs of Zika infection in adults – rash, fever, headache and body aches – are nonspecific, so a pregnant woman who develops such symptoms can’t be sure if she has contracted Zika or something less risky for her fetus.
A diagnostic test newly granted market authorization by the Food and Drug Administration (FDA) promises to help resolve this confusion. The test, developed by InBios International and based in part on technology licensed from Washington University School of Medicine in St. Louis, can detect signs of Zika infection in serum samples within 12 weeks of infection.
“Pregnant women living in or visiting places where Zika is endemic will want to know if they have been exposed to the virus,” said Michael S. Diamond, MD, PhD, a co-inventor of the technology that underlies the test. Diamond is the Herbert S. Gasser Professor of Medicine and a professor of molecular microbiology and of pathology and immunology at Washington University. “This test, along with another that detects viral genetic material at very early stages of infection, will help women and their doctors make informed health-care decisions.”
In 2016, Diamond and co-inventor Daved Fremont, PhD, a professor of pathology and immunology – along with then-graduate student Estefania Fernandez, MD, PhD, and postdoctoral researcher Haiyan Zhao, PhD – identified and characterized an antibody that detects Zika virus proteins. In the first days after infection, immune cells churn out large amounts of anti-Zika antibodies. The test uses Diamond and Fremont’s antibody – as well as other components – to detect anti-Zika antibodies in the blood of people recently infected with the virus.
Although the consequences of Zika infection are most severe for developing fetuses, in rare cases the virus also can cause serious illness in children and adults. It has been linked to brain swelling and to Guillain-Barre syndrome, a neurological condition involving muscle weakness and paralysis.
The test is not meant to be used as a stand-alone proof of infection. The FDA recommends that the test be used only for people with symptoms of recent infection, as well as a history of living in or traveling to geographic regions where Zika circulates. Positive results should be confirmed in accordance with guidelines from the Centers for Disease Control and Prevention.
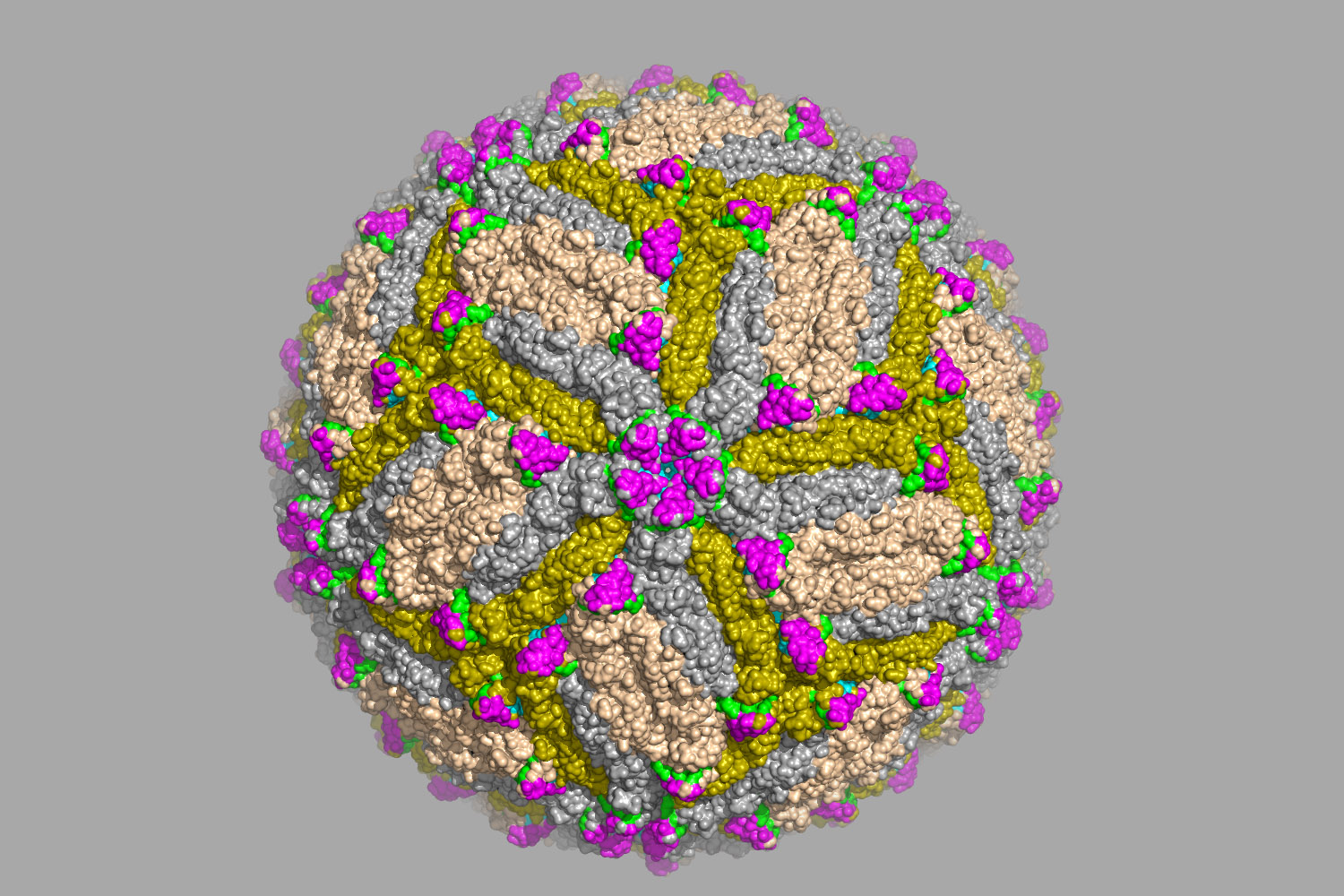 Related: Antibodies identified that thwart Zika virus infection
Related: Antibodies identified that thwart Zika virus infection
Could lead to vaccines, diagnostic tests and therapies







