Washington People: Sumanth Prabhu
Physician-scientist integrates patient care, innovative research on inflammation in heart failure
 Matt Miller
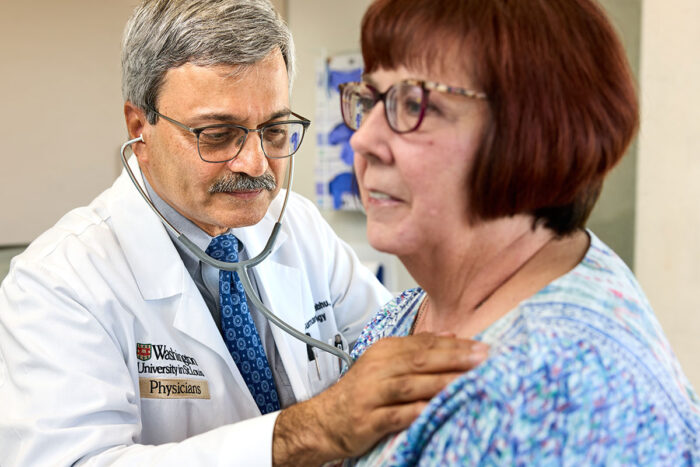
Matt MillerSumanth Prabhu, MD, director of the Cardiovascular Division at Washington University School of Medicine in St. Louis, uses a stethoscope to examine Pam Aydt, a patient in his practice. Prabhu is a heart failure specialist who combines his passion for patient care with his interest in understanding the role of inflammation in heart failure.
For Washington University cardiologist Sumanth Prabhu, MD, the stethoscope is not only indispensable as a diagnostic tool but presents powerful symbolism. He sees it as a channel that connects the patient to the clinician, a conduit through which a current of information flows from the former’s body to the latter’s brain.
“When you’re a trainee, there’s this tendency to use a stethoscope strictly as a tool,” said Prabhu, the Tobias and Hortense Lewin Distinguished Professor of Cardiovascular Diseases and director of the Cardiovascular Division. “You’re trying to master what your mentors are telling you about listening to the heart. But as you become a more experienced clinician, you learn how to use the exam, how to use your patient interactions and how to integrate these together. This connection is something that you never stop learning about.”
Prabhu, who also serves as cardiologist-in-chief at Barnes-Jewish Hospital, believes that the interactions he’s had with patients have been integral to shaping his work as a researcher studying heart failure, a condition in which the heart doesn’t pump blood as it should. Most recently, his lab at Washington University School of Medicine in St. Louis has concentrated on the underlying reasons behind, and triggers for, inflammation and immune cell activation in heart failure, and on finding new therapeutic approaches to alleviate inflammation and promote cardiac repair.
“We see many patients with inflammatory responses, for example, in heart failure,” Prabhu said. “In the laboratory, we’ve studied how modulation of inflammatory responses can set the failing heart along a path of improvement and recovery. The hope is that we can eventually introduce immunotherapeutics into the clinical management of patients with heart failure.”
Even in his teenage years, Prabhu knew that he wanted to pursue medicine, mainly because the science intrigued him. However, it wasn’t until the 1980s, when he enrolled in medical school and started doing clinical rotations, that the people side of medicine drew him in.
During this time, he found himself increasingly drawn to cardiology, in large part due to the personal attention and interaction required to assess patients and their hearts. Although the physical exam is not as precise as, for example, a cardiac MRI to evaluating heart function, it yields important information that allows clinicians to interact and bond directly with patients. Prabhu began to enjoy and value that connection.
He remained a scientist, though. Prabhu went on to develop a research program in heart failure at the University of Texas Health Science Center at San Antonio and then the University of Louisville School of Medicine, after which he became chief of the cardiology program at the University of Alabama at Birmingham.
With an ever-growing expertise in cardio-immunology, Prabhu arrived in St. Louis in 2021, when he was named director of the School of Medicine’s Cardiovascular Division.
At what point did you realize that you wanted to go into the medical field?
I’m the first doctor in my immediate family, but I realized I was interested in medicine very early on, when I was in high school. I think that when you’re young, a lot of that interest is driven by the scientific aspect of the field and the cool factor of what’s possible. As you move forward, it’s really the people aspect that becomes most important. The combination of that scientific perspective as well as the personal interaction with patients — both of those things were very appealing to me.
What drew your interest to cardiology?
Even as a medical student, I was just fascinated by cardiology. I went to medical school in the mid-1980s, when the field was seeing an explosion of new treatments and approaches. There were a lot of advances with medical therapy, and it was a field that was quantitatively very precise. It was all very exciting.
In cardiology, you can be uniquely involved with both science and people in very meaningful ways. It’s very individualized, I think. I was drawn to it very early on.
What have been some of the key challenges you’ve faced in this field?
On the research side, the challenge is always getting people to believe in your work, which is a healthy challenge, developing fruitful and long-lasting collaborations, and, of course, sustaining research funding. Cardio-immunology, for example, was a newly emerging field when I first started research in this area, and there was a certain bar and burden of proof that had to be met for the scientific community to accept the validity of new observations.
In terms of scientific discovery, one of the ongoing challenges is to rely more on multidisciplinary collaborations to develop innovations that can improve the lives of patients. For instance, in our efforts to understand heart failure, we need to combine efforts with our colleagues at other institutions, developing methods to gather and analyze data — such as patient outcomes, imaging studies and biopsy results — from multiple medical centers. Doing rigorous research on a grander scale across institutions and having enough funding to do it, I think, are very important issues facing the field. That’s also not something unique to cardiology.
Is there an important moment in your career that stands out to you?
Moving my research from cardiac remodeling and signaling to cardio-immunology in heart failure was a true watershed moment. The change was at once both incremental and extreme — I wanted a broader, integrative focus looking at how immune activation is driven by both cardiac injury and organs beyond the heart. This shift in focus to cardio-immunology was the culmination of many small steps driven from grassroots research principles; it took more than five years to publish our first paper on the immune remodeling of heart failure.
On the clinical side, it was really becoming a heart failure cardiologist as a logical outgrowth of my work with patients in general cardiology. There were no prescribed subspecialty training pathways for advanced heart failure and transplantation until the 2010s, well after I completed my fellowship, so I became a heart failure subspecialty cardiologist on the job, essentially, at the University of Louisville, where my partners and I were able to develop a high-volume destination left ventricular assist device (LVAD) program. I think this is one of the defining moments for me that thematically tied together my clinical and research expertise.
What do you think we can expect from the field of cardio-immunology in the future?
I think cardio-immunology is at an important crossroads, with discoveries being made at a rapid pace in multiple scientific areas, including heart failure, hypertension, atherosclerosis and cardio-oncology. As of now, most of this remains primarily in the preclinical space. The future — the next decade or so — is bright for clinical translation, moving from preclinical discoveries to clinical trials, and then ultimately into new therapeutic approaches to help patients.
How do you maintain work/life balance?
I should have mentioned that this is the biggest challenge; it’s more of a work/life integration.
My wife, Carolina Salvador, MD, is an associate professor of medicine in the Division of Oncology here at Washington University. She also directs the Integrative Oncology and Health Clinic at Siteman Cancer Center. Our daughter is now a senior at Dartmouth. Throughout our careers, we have needed incredible time-management skills to get things done at work and outside of work to have a healthy family life.
We have tried to set clear boundaries in terms of what’s family time versus what’s work time. It is difficult, I will say, as a cardiologist and physician to do this. Our profession is very demanding with sick patients often needing urgent care. And, being a physician-scientist, there are many deadlines for projects in the research lab that also demand attention. The support of my wife and family has been most important. The ability to delegate tasks to others, and to learn to prioritize your family and mental health, are very important.
What has surprised you about the School of Medicine, and your division in particular since your arrival?
WashU is widely known as an elite medical institution. But this reputation notwithstanding, I was still genuinely surprised at the incredible level of accomplishment of our faculty, across the clinical, research and teaching domains, and the strong scholarly ethos that permeates throughout the institution. WashU is really a special place for academic medicine.
Fast facts
Where did you grow up?
I grew up in the Northeast after coming here from India when I was very young. I didn’t leave the Northeast until I was ready to do my fellowship in cardiology. At that point, I went to San Antonio, Texas, for cardiology training.
Where did you go to college and medical school?
I did combined college and medical school training in Pennsylvania. I started off at Pennsylvania State University for my undergraduate degree, and then joined Jefferson Medical College — since renamed as the Sidney Kimmel Medical College — at Thomas Jefferson University for medical school.
Where did you do your training?
I did my residency at the University of Pittsburgh, and then went on to do a cardiology fellowship at the University of Texas Health Science Center at San Antonio.
What’s your favorite thing about St. Louis so far?
My wife and I love the city and its collection of different neighborhoods. I am very happy to be back in a town that loves Major League Baseball!







