Washington People: Benjamin D. Humphreys
Physician-scientist a leading innovator in kidney research
 Matt Miller
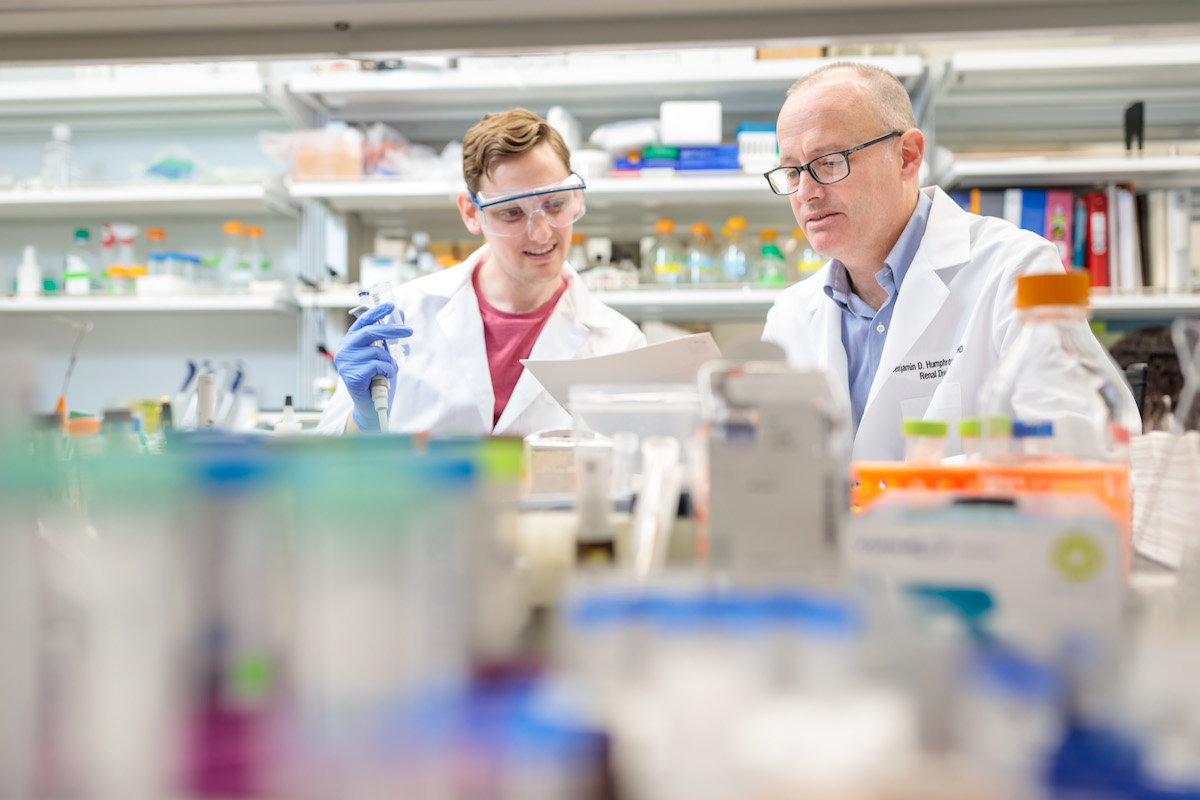
Matt Miller(Right) Nephrologist Benjamin Humphreys, MD, PhD, director of the Division of Nephrology in the Department of Medicine at Washington University School of Medicine in St. Louis, analyzes the quality of single cell RNA-sequencing libraries developed by Yoshiharu Muto, MD, PhD, a postdoctoral fellow in Humphreys' lab. A leading innovator in kidney research, Humphreys seeks to find better treatments to prevent kidney failure, a potentially fatal condition affecting 37 million Americans.
Benjamin D. Humphreys’ hobbies include experimenting with international cuisine in his kitchen, harvesting heirloom tomatoes in his backyard, and growing miniature kidneys in his laboratory.
He has been perfecting his first two hobbies for years. However, his interest in growing tiny kidneys — specifically, using human stem cells to cultivate kidney organoids — began in earnest in 2016, shortly after he was named director of the Division of Nephrology in the Department of Medicine at Washington University School of Medicine in St. Louis.
“It still amazes me that we can do this,” said Humphreys, MD, PhD, a noted nephrologist whose lab is funded by the National Institutes of Health (NIH). “This is the sort of cutting-edge scientific innovation that made me want to come here. Organoids are great models of kidney development and, potentially, kidney disease and transplant. There’s tremendous potential.”
Lab-grown organoids may one day help repair damaged kidneys or be used to test drugs aimed at fighting kidney failure, a growing problem in the United States, with more than 100,000 new cases annually. The potentially fatal condition affects 37 million Americans, most of whom don’t realize they have chronic kidney disease. No cure exists, and current treatments for end-stage disease mostly are limited to costly kidney transplants and dialysis.
“Ben Humphreys is an innovative and distinguished global leader in kidney research,” said Victoria J. Fraser, MD, head of the Department of Medicine and the Adolphus Busch Professor of Medicine. “Not only is he a brilliant physician-scientist, he is a generous collaborator and mentor.”
Humphreys earned a bachelor’s degree in English and American literature in 1991 from Harvard College in Cambridge, Mass., and his medical degree and PhD in physiology and biophysics in 2000 from Case Western Reserve University in Cleveland. He completed an internal medicine residency at Massachusetts General Hospital in 2002 and a nephrology fellowship at Brigham and Women’s Hospital in 2005. He was an associate professor at Harvard Medical School before joining the faculty at Washington University, where he is the Joseph Friedman Professor of Renal Diseases in Medicine.
What most interests you about the kidney?
The kidney is a fascinating, resilient organ. One of its characteristics that my lab studies is kidney regeneration. When a kidney suffers an acute injury, which might occur if you are ill and lose a lot of blood, the kidney has a powerful capacity to repair itself. Our hope is to harness this trait for therapeutic uses.
The kidney also is complex. The measure of its complexity is the number of different cell types that comprise it. There are more than 35 distinct cell types in a human kidney. It’s the body’s second most complex organ, behind the brain. However, the kidney’s function is simple. It’s a highly tuned responsive filter that dictates whether sodium, potassium, water and other substances need to be reabsorbed or secreted to keep the body perfectly in balance.
 Matt Miller
Matt MillerWhy aren’t there better treatments to prevent kidney failure?
There are several answers, but two are particularly important. The first dates back to the 1940s, when a physician named Willem Kolff invented the artificial kidney — the first artificial internal organ of any kind. It led to the life-saving procedure dialysis as we know it today. Patients with kidney failure die in about two weeks when dialysis is stopped. As wonderful as it is for the millions of patients saved by dialysis, one of the unintended consequences is the sense that kidney failure is a solved problem and, therefore, may not require as much investment because dialysis already exists. In fact, kidney research has been quite underfunded. For example, the NIH invests about $30 per patient for kidney-related research. However, for heart disease, the figure climbs to $60 per patient; and for cancer and HIV, it’s $500 and $3,000, respectively.
Besides an underinvestment in research, the kidney is complex. For example, type 1 diabetes is caused by the failure of a single cell type. By comparison, when a kidney fails, it’s 35 different cell types that have all collectively failed. Such intricacy makes it more of a challenge to develop new treatments. Adding to the complexity is that we don’t know yet — the keyword is “yet” — how to apply modern genomic technologies to classify broad categories of kidney disease into subtypes. In oncology, for instance, tumors used to be universally diagnosed by looking at a slide under a microscope. And if you had lung cancer, you’d look at the slide and all you could tell is whether it was a small-cell or nonsmall-cell tumor. But over the years, diagnostic precision has advanced. If a patient has lung cancer, a biopsy is taken, the genome gets sequenced, and it’s divided into 15 subcategories of the disease, all of which have specific responses to different drugs.
For kidneys, we are still at the stage where we’re diagnosing disease based on a slide under a microscope. This is not helpful for conditions such as diabetic nephropathy, a life-threatening chronic kidney disease that commonly affects people with diabetes. We know the condition behaves uniquely in different individuals; however, under a microscope, the kidney looks the same. We need to apply these genomic technologies to unravel the complexity and categorize diabetic nephropathy into disease subcategories. I’m most excited about the application of modern tools — not just genomics but computational biology, high-resolution imaging and the ability to study humans instead of mice — combined with using modern drug discovery and technologies to devise treatments. I believe we will enter a new era for our field within the next 10 years or so.
You earned an undergraduate degree in literature and then graduate-level science degrees. Did you originally consider a different career path?
I chose to major in English and American literature in college because I enjoyed reading and writing. It was not driven out of my anticipation of any future profession. However, about midway through my junior year, it hit me that I would graduate and needed to figure out what would happen next. I turned to science because I enjoyed physics and had been exposed to the field because my father was a nephrologist. One thing led to another, and I decided to become a doctor. But because I was an English major, I couldn’t fit all of my pre-med courses into the time remaining before graduation. I took a year to complete my requirements while also working as a research technician in a kidney lab. This was such a great experience that I decided to get an MD/PhD. My residency director and the chair of medicine were nephrologists and, with other physicians and scientists in the nephrology division, served as outstanding clinical and research role models and ignited my passion for nephrology.
How did your parents influence your career path?
I absorbed a lot from my parents. My mom has a PhD in French literature. She has spent her career in education at University of California, Berkeley — I grew up in the Bay Area — mentoring, recruiting and promoting roles for women and minorities, particularly in science and math. As for my father, I sometimes followed him on rounds. I admired his white coat and his compassion in caring for patients. But it wasn’t until after I finished my medical training that our professional relationship grew. We attended and presented research at scientific meetings together, including the annual American Society of Nephrology. We stayed in the same hotel rooms. More recently, my father, now a professor emeritus, has advised me on the challenges and opportunities of being a renal division chief since he was one at the University of California, San Francisco. The parallels go on.
You once won a scientific grant in a Shark Tank-style competition. Can you elaborate?
The competition was through the research arm at Brigham & Women’s Hospital, where I treated patients as a physician-scientist at Harvard Medical School. It was patterned after the ABC television show “Shark Tank,” in which entrepreneurs pitch business ideas to venture capitalists, or “sharks.” One of the guest judges was Kevin O’Leary, a shark on the actual TV show, known for his tough business acumen and his love of money. He’s nicknamed Mr. Wonderful. I gave a five-minute pitch on organ failure caused by fibrosis, or scar tissue. I was one of four scientists to win a $50,000 grant. The experience also proved valuable because it made me think about communicating my research to people who are not physicians or scientists. Researchers need to convince people what we’re doing is important because we need funding to develop new treatments.
 Courtesy of Benjamin Humphreys
Courtesy of Benjamin HumphreysCan you tell us about your family?
I’ve been married to my wife, Lisa, for 25 years. We met our sophomore year at Harvard. She’s a teacher, school counselor and a community advocate. I cannot overstate that I wouldn’t be where I am professionally without Lisa’s amazing support.
We have three children. My oldest son, Sam, is 20, and a sophomore majoring in finance at Washington University’s Olin Business School. Peter is almost 18 and a senior in high school. He enjoys math and science. Our daughter, Wendy, is 15, and a high school sophomore. She loves ice hockey. She and I spend hundreds of hours in the car on our way to hockey tournaments throughout the Midwest. I’ve coached all three of my kids in ice hockey even though I grew up in California.
We also have two Labrador retrievers: a black lab named Lewis and a chocolate lab named Lila. We’re all big dog people.
What are your other interests?
I enjoy cooking and gardening. I usually cook our family dinners on the weekends, and I especially love cooking for big holiday meals. I like experimenting with new recipes, and recently, I’ve been trying Korean dishes. Since moving to Missouri, I also have learned how to smoke ribs. I have a wifi-enabled thermometer that allows me to see my grill’s internal temperature in real time on my phone. I love data, so it’s perfect for me.
I enjoy flower and vegetable gardening, and I especially love growing heirloom tomatoes. I battle with the squirrels, though, who like to take one bite out of each tomato and leave the rest. That drives me up the wall.
I also like reading. Currently, I am reading Colson Whitehead’s “The Nickel Boys.” We were college classmates. What I really learned as an English major in college was how to write. That has served me well since I spend so much of my time writing grants and scientific articles. Being a good communicator is important in science.







