Study sheds light on parasite that causes river blindness
Data provides clues toward goal of eliminating worm infection
 Thomas Unnasch
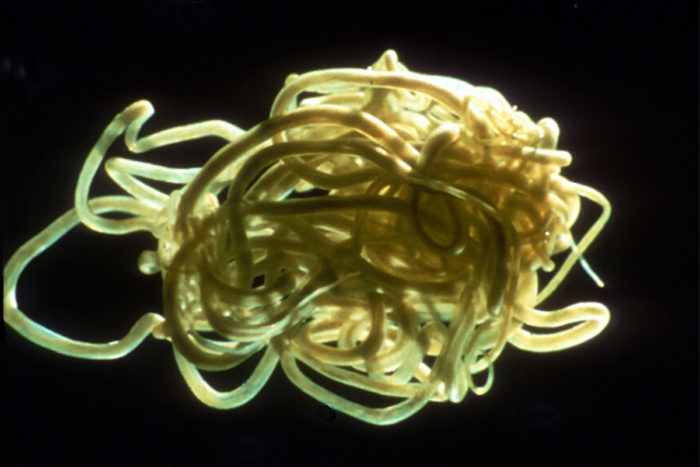
Thomas UnnaschPictured is a "nest" of the parasitic worm Onchocerca volvulus that causes river blindness. A new genomic survey of the parasite may provide clues to how the worm has become resistant to drug therapies.
The parasite that causes river blindness infects about 37 million people in parts of Africa and Latin America, causing blindness and other major eye and skin diseases in about 5 million of them. A study from Washington University School of Medicine in St. Louis sheds light on the genetic makeup of the parasite, a step toward the goal of eradication.
The study appears Nov. 21 in the journal Nature Microbiology, along with a companion paper also focused on the genetics of the parasite.
“In West Africa, there are two separate strains of this parasite based on geographic areas — the savanna strain and the forest strain,” said senior author Makedonka Mitreva, PhD, an associate professor of medicine. “The severity of the disease caused by each strain is very different. The savanna strains are much more virulent and have been associated with higher rates of blindness. The forest strains cause a mild skin disease. That’s why we wanted to see how they differ genetically.”
The parasite is a roundworm called Onchocerca volvulus and is carried by black flies that thrive near rivers and streams. Large-scale efforts to control the disease have been underway for decades, with mass drug-administration programs beginning in the 1970s in West Africa and in Central Africa and Central and South America in the early 1990s. The drug ivermectin remains the first-line treatment to target the parasite. The drug’s discoverers were honored with the Nobel Prize in Physiology or Medicine just last year.
With this treatment success combined with insect-control programs to reduce black fly populations, the World Health Organization (WHO) has set a goal of eliminating the river blindness parasite by 2025. But after several decades of exposure to ivermectin, these parasites are beginning to show resistance.
“We want to understand the origin of this resistance,” said Mitreva, who also is an assistant director of The McDonnell Genome Institute at Washington University. “Are these parasites evolving to survive the treatment, or are the surviving worms actually new strains that have been introduced due to migration of the black flies or of the parasite itself?”

To find out, Mitreva and her colleagues studied samples of the roundworms that have been stored since the early 1990s, before large-scale ivermectin treatment programs began. They also are sequencing present-day strains for comparison. The current study reports data only from the historical samples.
“We worked hard to find samples of the parasite that had not been exposed to the drug because we needed to establish an ancestral baseline,” Mitreva said. “The current worm populations and their genomes have been strongly shaped by 30 years of massive drug-administration programs. So you can’t just collect worm samples from these parts of the world today and sequence them. We had to look back in time.”
The new study included 27 roundworm samples taken in the early 1990s from four distinct regions — West African forest, West African savanna, Uganda and Ecuador. According to Mitreva, the Uganda strains, collected in central Africa, could not be classified as either the forest or savanna strain. Similarly, the strains from Ecuador, in South America, were also very different from the African strains.
Mitreva and her colleagues showed gene movement between the savanna and forest strains, but only in one direction. Genes from the savanna strain have flowed into the forest strain but not vice versa. This is due to differences in climate and the versatility of the black flies that carry the parasite.
“Black flies in the savanna region are known to survive in the forest region,” Mitreva said. “They can fly longer distances and live in the forest environment. But the forest black flies can’t survive in the savanna.”
The new study also included the complete genome sequence of a type of bacteria living in the parasite that the worm relies on for survival. Past evidence suggested that the more bacteria living in the parasites, the more severe the infection. But Mitreva said the current study does not support that observation. The investigators also are sequencing the same bacteria from present-day strains to see what, if anything, may have changed about them over the past three decades.
In general, Mitreva said, large-scale control efforts — including mass treatment with ivermectin and the use of insecticides to reduce black fly populations — have been very effective over the past 30 years. But since pockets of drug resistance are showing up, she said studies such as this one are important if the WHO’s goal of eliminating the parasite by 2025 is to be met.







