Seeking new guidelines for managing strokes with unknown time of onset
Washington University School of Medicine is participating in a trial looking at new treatment options for patients who have had a stroke with unknown time of onset
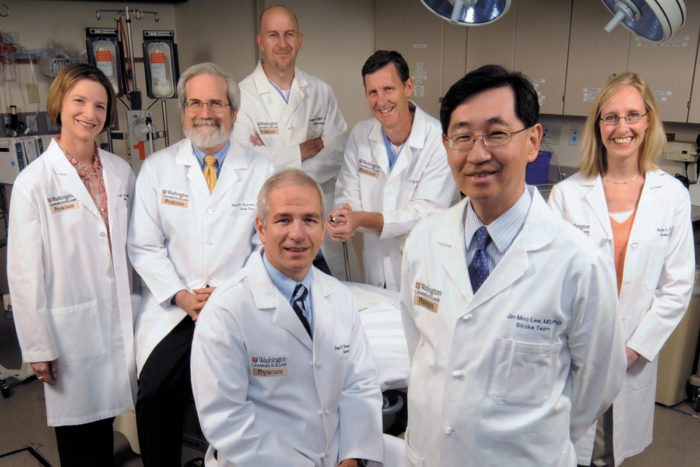
Washington University physicians at Barnes-Jewish Hospital treat 1,600 strokes annually, with four to 10 suspected stroke patients arriving each day. Members of the stroke team: (back row, from left to right) Renee Van Stavern, MD (neurology), David Carpenter, MD (neurology); Gregory Zipfel, MD (neurosurgery and neurology), Andria Ford, MD (neurology), and (front row) Peter Panagos, MD (emergency medicine and neurology), and Jin-Moo Lee, MD, PhD (neurology and radiology). Thanks to a new study by Ford, Derdeyn, Panagos and Lee, patients arriving with an unknown time of stroke onset may soon have more treatment options.
For stroke patients, timing is everything.
When doctors can pinpoint the time symptoms of a stroke begin, they have up to 4 ½ hours from that point to give the patient the anti-clotting drug, tPA. But when a stroke occurs while someone is asleep—what’s known as a wake-up stroke—the patient has no idea when symptoms began. For these individuals, tPA, or tissue plasminogen activator, is not an option under current treatment guidelines.
Washington University neurologist Andria Ford, MD, is working to change that. Ford is an investigator in MR-WITNESS, a phase II trial looking at safe administration of intravenous tPA in acute ischemic stroke patients who had unwitnessed onset of symptoms. This includes patients who had wake-up strokes, and also patients whose daytime strokes were not witnessed and who were unable to determine when their symptoms began.
To be enrolled in the trial, which began in 2011, a patient must arrive at the emergency department within 4 ½ hours of waking or being found. Upon arrival, the patient undergoes an MRI to determine when the stroke began. If MRI shows the stroke to be recent-onset (within the last 4 ½ hours), the patient receives tPA.
Using MRI to help reveal stroke onset
Although MRI has been shown in clinical trials to accurately determine the time of stroke onset, no previous trials have demonstrated the safety of intravenous tPA in patients who had unwitnessed symptom onset and later underwent MRI.
“Studies such as MR-WITNESS demonstrating the safety of tPA when MRI is used may be sufficient to allow a change in clinical care so that MRI can be used in this wake-up/unwitnessed onset stroke population,” Ford says.
Washington University is one of six enrolling clinical sites for the trial and has enrolled more than 25 percent of the total subjects in the study, Ford says. More than 50 patients have been enrolled so far across all six sites. The goal is 80 patients, and the trial is expected to conclude in 2016.
None of the study participants enrolled at Washington University have experienced adverse outcomes, according to Ford.
Because the trial is still enrolling patients, no results are yet available, but Ford described the promising outcome of one study participant: The 38-year-old woman awoke one morning with right-side weakness and aphasia. Her stroke was considered moderate to severe. Her MRI revealed that her stroke was recent-onset, so she was given intravenous tPA within an hour of her arrival at the emergency department.
“She had an excellent recovery, with a three-month disability scale of 1, indicating no significant disability due to her stroke,” Ford says.
She emphasizes that the eventual results of the MR-WITNESS trial might make this type of outcome possible for many others.
“Daily, we admit patients to our stroke service who either awoke with or had unwitnessed onset of stroke symptoms and who are automatically deemed ineligible for IV tPA. These patients have virtually no acute treatment options,” Ford says. “With completion of this study, it may be possible to identify a subset of these patients in whom it is safe to administer IV tPA, leading to less long-term disability.”
For more information on the MR-WITNESS trial, please visit the trial site on ClinicalTrials.gov.







