Proton therapy as effective as standard radiation with fewer side effects
Lower hospitalization rates following proton therapy could offset its higher upfront cost compared with standard radiation therapy
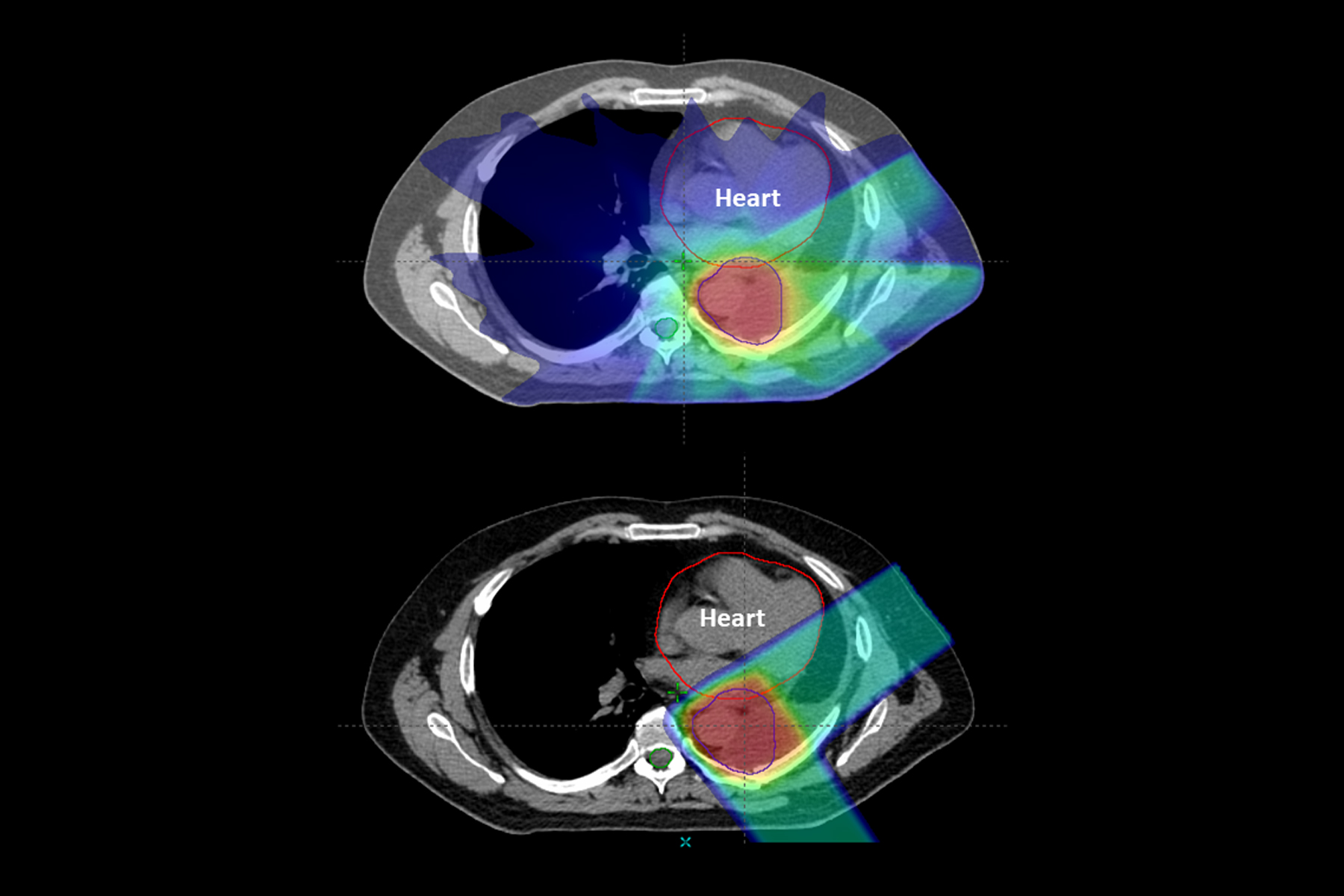
 Mevion Medical Systems
Mevion Medical SystemsA new study suggests proton therapy is as effective as traditional X-ray radiation therapy while causing fewer serious side effects. Pictured is proton therapy equipment at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine.
Cancer patients who receive high-tech proton therapy experience similar cure rates and fewer serious side effects compared with those who undergo traditional X-ray radiation therapy, according to a study led by Washington University School of Medicine in St. Louis and the Perelman School of Medicine at the University of Pennsylvania.
The reduction in side effects — particularly lower hospitalization rates and fewer emergency room visits — could offset the higher initial cost of proton therapy, which often is not covered by private insurance because of its higher upfront expense and limited data on its effectiveness compared to X-ray radiation, according to the researchers.
The study is published Dec. 26 in JAMA Oncology. Some of the findings also were presented in June at the American Society of Clinical Oncology’s annual meeting, in Chicago.
“We observed significantly fewer unplanned hospitalizations in the proton therapy group, which suggests the treatment may be better for patients and, perhaps, less taxing on the health-care system,” said first author Brian C. Baumann, MD, an assistant professor of radiation oncology at Washington University and an adjunct assistant professor of radiation oncology at Penn. “If proton therapy can reduce hospitalizations, that has a real impact on improving quality of life for both our patients and their caregivers.”
While radiation therapy can be curative for certain cancers, it also causes severe side effects — such as difficulty swallowing, nausea and diarrhea — that reduce quality of life and can, in some cases, require hospitalization, said Baumann, who treats patients at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine.
The study, which included almost 1,500 patients from Penn Medicine, is the first large review of data across several cancer types — including lung, brain, head and neck, gastrointestinal and gynecologic cancers — to show a reduced side-effect profile for proton therapy compared with X-ray radiation therapy for patients receiving combined chemotherapy and radiation. None of the patients had metastatic cancer, in which a tumor has spread to other parts of the body.
The researchers found no differences between the two groups in survival and cancer control, suggesting that proton therapy is just as effective in treating the cancer even as it caused fewer side effects. Overall survival at one year for the proton therapy group was 83 percent versus 81 percent for the X-ray radiation therapy group. This difference tipped slightly in favor of proton therapy but was not statistically significant.
The difference in side effects was more pronounced. Forty-five of 391 patients receiving proton therapy experienced a severe side effect in the 90-day time frame (11.5 percent). In the X-ray radiation therapy group, 301 of 1,092 patients experienced a severe side effect in the same period (27.6 percent). The patients receiving proton therapy experienced fewer side effects despite the fact that they were, on average, older and had more medical problems than those receiving standard X-ray radiation therapy. After taking steps to control for these differences, the researchers found that patients receiving proton therapy experienced a two-thirds reduction in the relative risk of severe side effects within the first 90 days of treatment, compared with patients receiving X-ray radiation therapy.
Both types of radiation therapy are approved by the Food and Drug Administration for cancer treatment. X-ray beams are made up of photons, which are electromagnetic particles that have almost no mass, allowing them to travel all the way through the body, passing through healthy tissue on the way out. Protons are relatively heavy, positively charged particles that hit their target and stop, essentially eliminating the exit dose of radiation.
Since the study found proton therapy to have fewer adverse events, Baumann said it could prompt radiation oncologists to design clinical trials to investigate whether increasing the dose of proton radiation would help patients do better, while still maintaining acceptable levels of side effects.
Similarly, the reduced side effects of proton therapy could allow older patients with additional medical conditions — who are typically excluded from clinical trials because of their frailty — to participate in trials investigating more intensive treatments that could be beneficial.
“Clinical trials often are limited to patients who have serious cancers but are otherwise quite healthy, and that’s not the real-world cancer population,” said Baumann. “Doctors, rightly, are concerned about toxicity. But with the reduced toxicity that we found with proton therapy, this might open the doors to the possibility of older patients with multiple medical problems getting cancer therapy they can tolerate that is more likely to be curative.
“With our aging population, this could have a big impact on a lot of patients,” he added. “To me, that’s an exciting implication of this research.”
 Brian Baumann/Mike Worful
Brian Baumann/Mike Worful






