Podcast: Giving stroke patients a hand
This episode of 'Show Me the Science' is about the IpsiHand, a device to help stroke patients use their brains to regain use of their hands
 Tamara Bhandari
Tamara BhandariMark Forrest shows off the fish he caught during a discussion of his work with the IpsiHand Upper Extremity Rehabilitation System. The device helped him recover use of his right hand following a stroke. After working with the IpsiHand, Forrest was able to build the fishing boat shown.
A new episode of our podcast, “Show Me the Science,” has been posted. In addition to reporting on the state of the COVID-19 pandemic, these episodes feature stories about groundbreaking research, as well as lifesaving and just plain cool work involving faculty, staff and students at the School of Medicine.
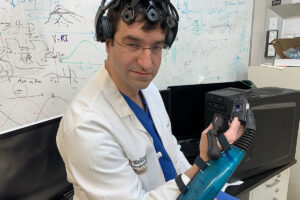
Brain-computer interfaces connect activity in the brain to an external device by means of a computer. Research has shown it’s possible to use such interfaces to move robotic arms and perform other tasks. Almost 30 years ago, Washington University researcher Eric Leuthardt, MD, a professor of neurosurgery, demonstrated that he could hook electrodes to the brains of epilepsy patients who were waiting to have brain surgery, and those patients then could play video games just by thinking about moving things on a screen. Over the years, Leuthardt’s team has learned to detect similar brain signals noninvasively. He co-founded the Washington University startup company Neurolutions Inc. to develop a brain-computer interface to help stroke patients recover function in their hands and arms.
In this episode, we learn about that device, known as the IpsiHand Upper Extremity Rehabilitation System. The IpsiHand involves a sort of cap that picks up brain signals from a stroke patient and transmits the signals to an exoskeleton fitted over the patient’s paralyzed hand. While wearing the system, patients think about moving the affected hand, and the IpsiHand translates that intention into actual hand movement.
 Elizabethe Holland Durando
Elizabethe Holland DurandoOver time, the patient’s brain slowly learns how to move the hand by itself. In addition to Leuthardt, we’ll also speak to a man who helped test an early version of the device years after a stroke left him unable to use his right hand. After working with the IpsiHand, the stroke patient, Mark Forrest, regained enough use of his right hand that he was able to build himself a boat. We’ll ride on that boat with him as he catches some fish and discusses his recovery.
The podcast, “Show Me the Science,” is produced by the Office of Medical Public Affairs at Washington University School of Medicine in St. Louis.
Transcript
Jim Dryden (host): Hello, and welcome to “Show Me the Science,” conversations about science and health with the people of Washington University School of Medicine in St. Louis, Missouri … the Show-Me State. During the first two years that we produced this podcast, we focused entirely on how the School of Medicine doctors, researchers and trainees responded to the COVID-19 pandemic. Now as the pandemic, we hope, is receding just a little, we also are reporting on some of the other research, lifesaving and just plain cool work being done at the School of Medicine, and this topic certainly qualifies. In this episode, we’ll tell the story of a device developed at Washington University School of Medicine that can help people who have been disabled by stroke regain significant control over their arm and hand function by using their minds. And we’ll hear from one such patient. Mark Forrest had a stroke in 2015. More than two years later, and after his therapists had told him he had regained about as much function as he was going to, Forrest participated in research involving the IpsiHand, which allows patients to use signals from their brains to activate a device on their arms that helps them regain hand movement. We talked to Forrest recently as we sat on the fishing boat that he built himself after recovering some use of his right hand.
Mark Forrest: You got to think about what to do. It’s just not a hand piece that works by itself. It’s through your mind. You have to think about what you’re doing to make it work. So that’s what I did, and it helped me out a lot because it made my hand move a lot faster, a lot better.
Dryden: For more than two years, Forrest’s right hand was balled into a fist. He couldn’t move his fingers or use his right arm. It’s still not perfect, but the combination of his determination and his use of the IpsiHand device has him doing things that were impossible not that long ago. My colleague, Tamara Bhandari, came with us on the boat ride. She’s written extensively about the IpsiHand, and she’s here now with some background about where this FDA-approved device came from, how it was developed and what it might mean going forward. So, Tamara, this whole thing comes from the work of Washington University neurosurgeon Dr. Eric Leuthardt, correct?
Tamara Bhandari: Well, Dr. Eric Leuthardt and also Dan Moran, who’s an engineer in the McKelvey School of Engineering here at WashU. Early in his career, Dr. Leuthardt was working with Dr. Moran on some projects involving brain-computer interfaces. And then from those projects, that’s where they started to get the ideas that grew into the IpsiHand. And the two of them founded Neurolutions in 2007, which is a company to develop brain-computer interfaces.
Dryden: And the IpsiHand is designed for people who in the past would have been thought to have pretty much recovered about as much function as they were going to recover, right?
Bhandari: Right. So they’re called chronic stroke patients. So more than six months after your stroke, you become a chronic stroke patient. In the immediate aftermath of a stroke, people recover some function. Some of that is spontaneous, some of that can be helped with therapies. But after about six months, it tapers off. And so what Dr. Leuthardt realized was that you don’t actually have to stop at that point, that the brain is still plastic, you can still recover and relearn some of those functions that you used to have.
Dryden: And it works.
Bhandari: Yes, it works. And it works by retraining the brain. So it’s a little different from other brain-computer interfaces that other people have been developing that you might have heard about where they use their brains to, for example, move a prosthetic arm. It’s not like that. They’re actually training their brain to develop these functions so that after you’re done wearing the IpsiHand, your brain can control your hand by itself. And that’s why they got a breakthrough designation from the FDA, which means that this was an innovative solution to an unmet need. So that tells you that this is really new and it’s really important.
Dryden: To learn more about brain-computer interfaces, we went straight to the horse’s mouth.
Eric Leuthardt, MD: Hi. My name is Eric Leuthardt. I’m a professor of neurosurgery and engineering at Washington University and the chief of the Division of Neurotechnology.
Dryden: As a college undergraduate, Leuthardt studied biology and theology, and he’s always been interested in mind-body connections, which eventually led him to study brain-computer interfaces, experiments where he demonstrated that people could play video games using only their brains, no hands required. They literally could play video games just by thinking without touching anything at all.
Leuthardt: It started with an appreciation. I remember Dan Moran — kind of my mentor at the time, he’s a professor of engineering — and I were sitting down, and we were planning the research that I was going to do during my training. And initially, we were talking about how we’re going to record electrodes in mice and look at mouse brain signals. And we started to talk about the fact that, well, wait a minute, there is a clinical scenario where humans have electrodes in their brains. Very specifically, this is in the setting of intractable epilepsy where, for a period of time, patients who have really bad seizures, to figure out where their seizures are coming from, you basically do a surgery where you make an incision in the scalp, you take a window bone off the skull, you implant electrodes on the surface of the brain, you put that skull back and you close the scalp up. And they have these electrodes that are recording their brain activity for about one to two weeks. And during that time they’re really just sitting there. But that time in between their procedures is really this unique golden opportunity to record brain signals from human subjects in a way that you really couldn’t do otherwise. And so that was the aha moment for Dan and I to say, “Well, wait a minute, why don’t we try to use those windows of time to study brain physiology?” And that’s where we started to think about, “OK, well, what do we want to study? What do we want to do?” From a brain-computer interface standpoint, the most straightforward thing to think about is motor movements. We know where motor cortex is, that’s pretty easy to identify. And motor movements is something you can really measure. Do they open and close their hand? Do they move their hand in space? And these are things we could really map out in the real world and then map it back into the brain signals.
Dryden: At what point does this work become, we can make a device that could help people who can’t do some of those things?
Leuthardt: Well, fundamentally, the goal was always to create something to help patients with motor disabilities. And this becomes a long journey in the sense that as we really started to show that we could decode signals from the brain, we could have people control cursors on the screen, we could have them control robotic arms, we thought, “Oh, my goodness, this is going to be a really great opportunity to help people.” What we initially envisioned was people with severe motor disability, who have quadriplegia, people who are paralyzed. Because the brain is intact, but either they have a spinal cord injury — they’ve got a spinal cord injury where they can’t move — or, for instance, examples like ALS (Lou Gehrig’s disease), where their muscles aren’t controlled by their spinal cord anymore. And so we started a company. It was called Neurolutions. Our initial vision was to create this really small implant that we could put over motor areas. Both Dan and I were extremely committed. We wanted to make brain-computer interfaces a reality for patients. And so that got us thinking about what’s the biggest source of motor disability in the world right now? And it’s stroke. And that’s where we started to explore, well, again, a stroke patient can still think about moving their hand even though they can’t move it. Where do those brain signals live if the main part of the motor area, that was classically understood, is gone?
Dryden: Here we need a quick refresher to remind that, in general, movement in the right side of the body will be controlled by the left side of the brain, while the body’s left side is linked to the brain’s right side. But as the research continued, Leuthardt’s team discovered that sometimes the brain can affect movement on the same side of the body, which brain mappers call the ipsilateral side.
Leuthardt: And as it turns out, that was a really rich area of discovery. We really learned and understood how the brain does have brain signals associated with same-sided limb movements. And some of those signals are represented in low frequencies. The reason that that is important is because if you can imagine when you’re listening to music through a wall, the high-frequency stuff you can’t hear, but the low bass you can hear. Similarly, when you think about your brain inside your skull inside your scalp, those low frequencies you can pick up noninvasively. And so now we’ve got the ability to pick up signals noninvasively. So it doesn’t require surgery anymore. We can pick them up just by putting electrodes on the scalp. And because it’s ipsilateral, it’s on the uninjured side of the brain, we can now create kind of a system where it’s noninvasive, it’s a headset. And now a stroke patient could potentially control this and potentially provide some utility. So we discovered that we could pick up those signals noninvasively. We could have these stroke patients control signals with their brain. And that led to the next jump. We said, “Ok now, if these patients can use that unaffected side of their brain to control something, can we create a wearable exoskeleton that can actually allow them to control their hand?” And so that led to the next round of discovery where we created not just the method that we can pick up these signals, but actually, this system where basically we now have a wearable headset and it’s connected to this wearable exoskeleton that has all the computing power to basically process the brain signals, use those brain signals to control this wearable that opens and closes a stroke patient’s paralyzed hand. We not only wanted them to control that hand, we kind of took it to the next level. We said, “OK, if that uninjured side of the brain is controlling the paralyzed hand, does it cause the brain to rewire?” So that basically now that uninjured side of the brain is no longer just associated with the thought and the imagination to move, it’s actually controlling it. Can that actually take over some control if they actually use it for a long period of time? And so we put that to the test in a pilot feasibility clinical trial. And again, our first 10 subjects did great.
Dryden: Using the device, Leuthardt says, might be compared to weight training. Using it a few times a day for a few months would strengthen the links between the affected side of the body and the unaffected side of the brain. That’s what stroke patient Mark Forrest did as Leuthardt’s team and his company were developing the IpsiHand. Patti Forrest, Mark Forrest’s wife of 45 years, picks up the story.
Patti Forrest: And we were very keen on the fact that it’s the first six months, they tell you, to a year when you see improvement. And he worked so hard and so continually for that first year, and there was very little improvement. I mean, a little, enough that he could kind of get around, but his hand was basically kind of stuck. And he went to a physical therapist, and he became friends with her, and she saw how hard he was working, and he asked her if she would tell him whether he would get any better after that. He asked her for an honest answer and she said, “No, I don’t think so.”
Dryden: But rather than quit when bad news arrived, Forrest remained determined and a symbol of that determination now regularly floats on a farm pond as Forrest fishes that pond, which is about 80 miles from St. Louis.
Mark Forrest: I was determined not to be perfect, but I wanted to be better so I had usage of that hand and leg and be able to do things on my own and don’t expect people do it for me. Because that’s the way I am. My last therapist I had before I left the hospital, she told me, honestly, I’m done. It won’t get any better. So as I told you, I got in my car, had a good cry, and said, “I’m going to prove everybody wrong.” So I did. I just kept working on it. Even to this day, it’s been seven years, and I’m still doing exercises trying to get better and better.
Dryden: As we sit here on this boat, on this lake, was this one of the things that drove you to want to get better, to be out here in the peace?
Mark Forrest: Yes, because the boat we were using at the time, the transom on that boat was getting bad, and I was going to have to replace it. So I decided rather than replace it, to build a new boat. And we’re sitting on it now. I mean, this boat wasn’t a plan that I bought. This boat was in my head and I decided, “Damn it, I don’t care if I had a stroke or not, I still want to fish this place.”
Dryden: And fish he did. During an hour on the water, Forrest caught a whole bunch of fish, throwing all of them back and allowing himself to try to catch them again on his next trip. He is not a man who does things halfway, which is a trait he also applied to his work with the IpsiHand.
Mark Forrest: They said they wanted me to do it once or twice a day. Well, that didn’t happen with me. It usually takes an hour to do a session. I would do a session and then take an hour break and do another session, take an hour break, and I would do that all day long. I could literally walk around and do things and still do the program with the hand. And all you’re doing is thinking about it. So all I do is think and then do it.
Dryden: Right because the idea of the device is that your brain is sort of —
Mark Forrest: Your brain has to move it. OK. Even though you know what the device is going to do, you still have to think about it to let it do it. So it’s not like the machine takes care of it, because it doesn’t. Your mind is still working to get your hand to work.
Dryden: Neurosurgeon and IpsiHand inventor Eric Leuthardt compares a stroke patient using the device to an athlete using training equipment.
Leuthardt: This is a system that you use, that really you train with. The way it was defined for the initial trials is at least once a day, five days a week, for three months, and that creates tangible benefits. And importantly, those benefits are durable, meaning that we also looked at our patients six months out after they complete it, and they still maintained those functional improvements. I think it’s an open question of how much do you continue to train? And that’s some of the science that we will continue to do is that, as people use it for longer and longer periods of time, do they gain more? Do their muscles, their cognitive or brain muscles get stronger over time? That’s questions we’re still working to answer. Clearly, it’s a short rehabilitation solution that is helping people where there weren’t solutions before, but what’s the plateau? And we’re still trying to figure that out.
Dryden: And with this technology, you are taking advantage of brain that has not been damaged. Stroke patients recover for a few months, and then recovery ends, for most anyway. So this is something that would be available to folks who might have had a stroke 10 years ago.
Leuthardt: It’s absolutely intended for chronic stroke patients. And the dogma at the time was that, look, there’s a three- to six-month window after stroke, where typically people say if you haven’t recovered function at that point, that’s what you’ve got. And we really set to challenge that paradigm. The system is really, we believe, inducing plasticity. It’s letting the brain remodel a network in a way that is essentially allowing you to recover function with the uninjured parts of your brain.
Dryden: And Leuthardt says he can foresee using a device like the IpsiHand in the clinic as well as at home as more stroke patients are treated using telemedicine. It’s been engineered so that it can be attached by the patient with one hand, which is important because it’s designed to help stroke patients who only have use of one hand.
Leuthardt: Now, I think what makes the IpsiHand and our technology special and exciting, in my opinion — well, first off, it was the first FDA-approved brain-computer interface for motor disability, full stop. And I think that that is really kind of a sea change. And again, we were very fortunate in getting that breakthrough designation and really working closely with the FDA as we worked through getting that FDA approval because they held us to a high bar and I’m glad they did.
Dryden: Seven out of those first 10 patients that were in the trial had good results in that when they were not using the device anymore, they had more use of the injured part of their body. Is that what that meant?
Leuthardt: Yes, that’s correct. There are prompts, and there’s kind of a whole paradigm where they would use their intent to control their hand, and they would control their hand. And those patients showed really robust improvements in their hand function. I’d say more importantly and somewhat anecdotally, these metrics translate to really impactful things that affected these patients’ lives. So I just very clearly remember, for instance, I was walking down the hallway at one point and one of the patients flagged me down and said, “Dr. Leuthardt, Dr. Leuthardt, I just want to let you know that I can put my pants on for the first time in three years.” And it’s one of these moments where you do the science, you publish the papers, and you got to do a lot of cerebral, intellectual things, and you’re excited about them. But this was a deeply emotional thing for me where suddenly you realize, OK, this kind of concept that I had, it translated to something so fundamental that, really, it kind of impacted this man’s dignity. And it was and it still is one of the most important academic moments in my career, where you realize something that you invented is really having a new way of helping somebody. And that, for me, was one of the big moments. And there’s a number of stories like that.
Dryden: Including the story of a man named Mark Forrest, who after his stroke in 2015, never gave up hope that he could go out and fish again. He even built his own boat. But he still has some goals that he hasn’t yet achieved.
Mark Forrest: What are you going to do? Cry about it? Or are you going to make it work better? So I don’t cry. I mean, I cry because of the aggravation of having to do this and work hard at it, but it’s life.
Dryden: You said on the way out here that one of your goals now that you’ve gotten movement back in your right hand, is that you want to be able to cast that rod with your right hand.
Mark Forrest: I’m going to throw that rod one more time before I die with my right hand, and I am determined to do it. It’s going to still take time. It won’t happen overnight, but I’m going to do it. I built this damn boat. I better make sure I can make my hand work right.
Dryden: The IpsiHand, which is FDA-approved, should soon be commercially available to assist stroke recovery patients at several centers around the United States. “Show Me the Science” is a production of the Office of Medical Public Affairs at Washington University School of Medicine in St. Louis. The goal of this project is to introduce you to the groundbreaking research, lifesaving, and just plain cool work being done by faculty, staff, and students at the School of Medicine. If you’ve enjoyed what you’ve heard, please remember to subscribe and tell your friends. Thanks for tuning in. I’m Jim Dryden. Stay safe.







