Persistent childhood asthma sets stage for COPD
Lifelong attention may be needed to prevent worsening lung function
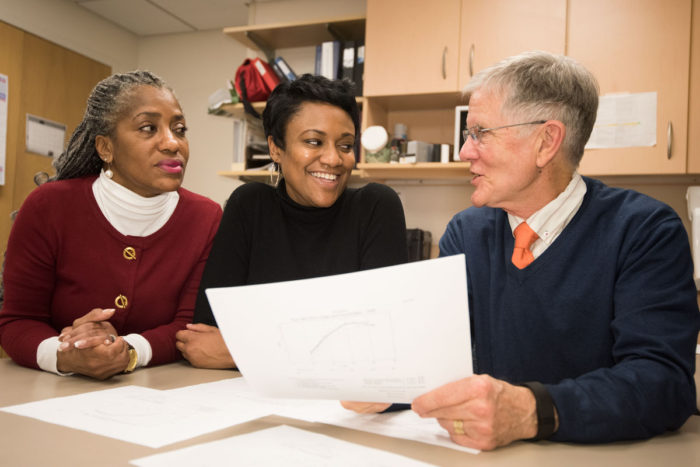 Robert Boston
Robert BostonRobert C. Strunk, MD, (right) discusses results of a decades-long pediatric asthma study that involved Janae Smith, (middle) a patient and study participant, and Denise Rodgers, (left) who retired earlier this year as a clinical research coordinator. The findings emphasize that lifelong attention may be needed to prevent worsening lung function. Strunk, a renowned pediatric allergist, died of cardiac arrest April 28, before the new study's publication May 12 in The New England Journal of Medicine.
Children with mild to moderate persistent asthma are at greater risk of developing chronic lung disease as young adults and, therefore, may require lifelong treatment even if their asthma symptoms subside for extended periods, according to a major national study.
The study – led by researchers at Washington University School of Medicine in St. Louis, Brigham and Women’s Hospital in Boston and Harvard Medical School – is published May 12 in The New England Journal of Medicine.
Researchers tested lung function and development in 684 children with asthma during a two-decade span beginning in the mid-1990s, when participants were ages 5 to 12. The results showed that 75 percent of the participants experienced abnormal lung growth patterns by early adulthood that increased the likelihood of developing chronic obstructive pulmonary disease (COPD), a progressive condition that makes breathing difficult and has no cure.
“It is astonishing,” Robert C. Strunk, MD, the Donald B. Strominger Professor of Pediatrics at Washington University School of Medicine, said in an interview earlier this year before he died of cardiac arrest April 28. “For people barely into adulthood to already have COPD is terrible. As the disease evolves, they are likely to have health problems that will make it difficult to participate in normal day-to-day responsibilities such as holding a job.”
Co-senior author Scott T. Weiss, MD, a professor of medicine at Harvard who treats patients at Brigham and Women’s Hospital, stressed the importance of identifying at-risk children early and counseling them about preventive measures. “Since asthma itself is a risk factor for developing COPD, these patients should be advised against risk-related environmental exposures, like smoking, that could intensify their symptoms and increase their COPD risk,” Weiss said. “It is important that we recognize this link between persistent childhood asthma and COPD as a potential problem and focus on prevention efforts.”
The findings stem from the Childhood Asthma Management Program, or CAMP, a study of 1,041 U.S. patients. The study’s aim was to identify the best way to treat chronic childhood asthma. Earlier data from the study – first published in The New England Journal of Medicine 16 years ago — changed the standard of care for pediatric asthma after research showed that regular medications were more effective than as-needed asthma treatments.
Through the years, the team has followed just over three-fourths of the CAMP children into their mid-20s, gathering more than two decades worth of data that led to several landmark studies.
“Thanks to the dedication of CAMP patients, we have learned a lot about pediatric asthma management,” said Strunk, who treated patients at St. Louis Children’s Hospital for many years.
Using a spirometer to measure how much and how quickly a patient can exhale, researchers found that nearly half of the participants had reduced lung function development as young adults, increasing their risk for developing diseases such as chronic bronchitis and emphysema.
Data also determined that males develop more asthma-related, long-term lung problems than females.
Despite numerous advances from the CAMP study, Strunk said many unknowns still exist about asthma. “The main issue is that mild to moderate persistent childhood asthma does have lifelong consequences,” he said. “As with most studies in clinical medicine, we do not have a final answer on what can be done to change the clinical course, but the disease must be taken seriously by families and treated to minimize symptoms and maximize lung function.”
Strunk cautioned that teenagers and people in their 20s should maintain asthma treatment even if the disease stabilizes for several years, “a period known as the plateau of lung function” that often precedes gradual lung function decline.
“It’s important for patients, families and physicians to keep asthma management at the forefront,” Strunk said. “Families must minimize exposure to irritants such as cigarette smoke, pet dander and mold, to which asthmatic children are particularly sensitive.”
Janae N. Smith entered the CAMP study in 1994, when she was a 10-year-old with chronic asthma. With Strunk’s help, she removed potential asthmatic triggers and maintained treatments. “Not being able to breathe is really scary because you never know what can happen,” said Smith, who is now a clinical nurse coordinator for the School of Medicine’s Department of Medicine. “My asthma attacks used to come on without any warning and then escalated really quickly. It was a horrible experience.
“I still have asthma now,” Smith said. “However, it isn’t anywhere near as severe as it was when I was a child, largely due to how I was taught by Dr. Strunk to manage the disease.”







