NIH awards 4 medical school scientists prestigious ‘high-risk, high-reward’ grants
Richards, Laidlaw, Orvedahl, Shmuylovich chosen for their innovative research projects
 Washington University School of Medicine
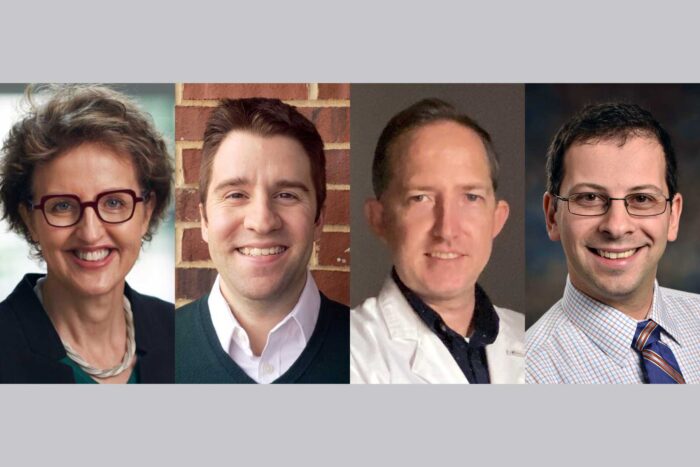
Washington University School of MedicineFour researchers at Washington University School of Medicine in St. Louis have been awarded "high-risk, high-reward" grants from the National Institutes of Health (NIH). The grant program aims to inspire scientific discovery by providing support for highly innovative research. The grant recipients are (from left) Linda J. Richards, PhD; Brian J. Laidlaw, PhD; Anthony W. Orvedahl, MD, PhD; and Leonid Shmuylovich, MD, PhD.
Four scientists at Washington University School of Medicine in St. Louis have been awarded prestigious grants from the National Institutes of Health (NIH) aimed at supporting the researchers’ innovative and impactful biomedical and behavioral research.
The grants are among a total of 106 such grants awarded to scientists recognized via the NIH Common Fund’s High-Risk, High-Reward Research program. The program aims to spur scientific discovery by providing support for highly innovative proposals that, due to their risk, may face hurdles in the traditional peer-review process. The 106 awards total about $329 million over five years, pending availability of funds.
The School of Medicine’s grant recipients are: Linda J. Richards, PhD, awarded an NIH Director’s Pioneer Award; Brian J. Laidlaw, PhD, and Anthony W. Orvedahl, MD, PhD, each awarded an NIH New Innovator Award; and Leonid Shmuylovich, MD, PhD, given an NIH Director’s Early Independence Award.
Richards, the Edison Professor of Neurobiology and head of the Department of Neuroscience, has received the Pioneer Award, an award that challenges investigators at all career levels to pursue new research directions and develop groundbreaking, high-impact approaches to areas of biomedical, behavioral or social science.
Her award will support research focused on a new animal model for studying early brain development. She is using the fat-tailed dunnart, a small mouse-sized marsupial, to understand how the brain first switches on. Placental mammals such as mice and people are born with basic brain wiring and organization in place. But marsupials are born at relatively early developmental stages. Developmentally speaking, a newborn dunnart’s brain is equivalent to the brain of a human fetus at 7 weeks’ gestation, or a mouse’s brain at 10 days’ gestation. Consequently, many of the key processes that shape the brain occur before birth in mice and people but after birth in dunnarts, giving scientists the opportunity to study brain development at its early stages.
“We’ve done a lot of work developing this animal model, demonstrating that many of the basic processes are the same in mouse and dunnart,” Richards said. “Now we’re ready to start using it to answer questions. We want to know how the brain first switches on, how the circuits develop that allow coordinated patterns of activity across the brain, and how that underpins brain function and behavior.”
With the support of the Pioneer Award, Richards plans to study patterns of neural activity and trace the circuits that connect brain cells within networks.
“This is very fundamental research,” Richards said. “In the past, we haven’t had a way to study these early events, so there’s an enormous amount we don’t know about how the brain develops and what that might mean for neurological and psychiatric conditions that occur later.”
Richards earned her bachelor’s degree at Monash University in Melbourne, Australia, and a bachelor of science with honors and a doctoral degree at the University of Melbourne, through the Walter and Eliza Hall Institute for Medical Research in Melbourne, before moving to San Diego for postdoctoral studies at the Salk Institute for Biological Sciences. She took her first faculty position at the University of Maryland School of Medicine, where she focused on molecular genetic mechanisms of brain development. In 2005, she moved back to Australia to take a faculty position at the Queensland Brain Institute. She became deputy director of research within the institute in 2015. She joined Washington University as head of the Department of Neuroscience in January 2021.
Laidlaw, an assistant professor of medicine in the Division of Allergy and Immunology in the Department of Medicine, received an NIH New Innovator Award, which supports unusually innovative research from early-career investigators who are within 10 years of their final degrees or clinical residencies. The award provides $300,000 per year in direct funding for five years.
The Laidlaw lab studies the development of immunological memory. He and his lab members are interested in the development and function of memory B cells, a type of immune cell that helps the body protect against viruses or other invaders that the immune system has been exposed to in the past, either through natural infection or vaccination. His lab uses mouse models, genetic sequencing and genetic screening techniques to identify how immune memory develops and operates in disease states.
His work is focused on overcoming a natural bottleneck in the number of memory B cells that develop following a viral challenge. Overcoming that bottleneck could lead to the development of vaccines that can induce a more broadly protective immune response. Laidlaw also is interested in understanding how memory B cells develop in mucosal tissues, such as the lungs. There, many viral infections take hold, including influenza and coronaviruses. Developing vaccines that can induce memory B cells at the site of infection is important in protecting against rapidly mutating viruses that can cause breakthrough infections.
Conversely, Laidlaw is interested in understanding situations where memory B cells play a role in causing disease, such as in allergy and autoimmune disorders.
“I’m honored to receive the NIH New Innovator Award,” Laidlaw said. “I look forward to the opportunity to bring new students and researchers into my lab and build on our work into understanding the development and function of memory B cells.”
Laidlaw earned his undergraduate degree in biochemistry from the University of Pennsylvania in 2011. He continued his studies at Yale University, earning his doctoral degree in 2015. Before joining the faculty of the School of Medicine in 2020, Laidlaw was a Damon Runyon Postdoctoral Fellow at the University of California, San Francisco.
Orvedahl, an assistant professor of pediatrics, and of pathology & immunology in the Division of Pediatric Infectious Diseases, received an NIH Director’s New Innovator Award to support research exploring how the body’s immune system reacts to infections, including the virus that causes COVID-19. The aim is to control cellular activity that can cause a life-threatening inflammatory overreaction known as a cytokine storm.
Cytokines are molecules released by certain cells in response to infection. Sometimes, cytokine production uncontrollably veers into overdrive — a reaction that can lead to organ damage or death. Orvedahl’s studies, in mice, revealed a potential antidote to the cytokine storm through autophagy, a natural process in the body that eliminates cellular waste to allow for the regeneration of newer, healthier cells. Autophagy genes maintain the survival of an important cell type known as macrophages against two key cytokines, interferon and TNF (tumor necrosis factor), that have been implicated in COVID-19-associated cytokine storm.
Orvedahl and his research team plan to develop novel tools to study the moment that virally infected lung cells alert the immune system’s first-responder macrophage cells. Although these early events are thought to be important in setting the stage for whether an infection is mild or severe, the exact identity of factors that lead to these widely variable outcomes are not well understood. Specifically, the team will use high-precision gene-editing tools such as CRISPR to generate a cellular road map of the lungs of mice infected with SARS-CoV-2.
“Using this system, we will seek to understand how the cytokine conversation breaks down between SARS-CoV-2-infected lung cells and their neighboring macrophages,” Orvedahl explained. “Our studies will focus on the role of the autophagy pathway, but we will also develop unbiased screening tools to identify novel genes in both respiratory cells and macrophages.”
Orvedahl earned his medical degree and doctorate from the University of Texas Southwestern Medical Center in Dallas in 2012. He then trained for two years as a pediatrics resident at St. Louis Children’s Hospital and for four years as a fellow in pediatric infectious diseases at Washington University through the Accelerated Research Pathway program. His postdoctoral research was under the mentorship of Gary Silverman, MD, PhD, the Harriet B. Spoehrer Professor and head of the Department of Pediatrics, and Herbert “Skip” Virgin IV, MD, PhD, the former head of the Department of Pathology & Immunology. Orvedahl joined the faculty in 2018.
Shmuylovich, an assistant professor of medicine, of pediatrics, and of radiology, has received the NIH Director’s Early Independence Award. This award provides support for outstanding junior scientists to bypass the traditional postdoctoral training period and launch independent research careers.
The pediatric dermatologist’s work is focused on developing imaging tools to objectively measure skin disease at large and small scales in diverse skin types. Doctors often diagnose skin disease by sight, but signs of skin disease can be subtle in pigmented skin, leading to systemic underdiagnosis and undertreatment in patients of color. The Shmuylovich lab is addressing these problems by developing short-wave infrared imaging devices.
“My goal is to leverage the power of infrared imaging to make these subtle findings much more obvious and allow for more objective assessment of skin disease in kids and adults with diverse skin types,” he said.
Short-wave infrared light offers a window into skin disease that is independent of skin pigmentation. Recently, Shmuylovich showed that short-wave infrared imaging can be used to visualize and quantify skin inflammation. Short-wave infrared light also travels deeper through skin than visible light, which makes it possible to build a device that provides a noninvasive alternative to skin biopsy at imaging depths greater than existing microscopic skin imaging devices.
With the support of the Early Independence Award, Shmuylovich aims to bring short-wave infrared macroscopic and microscopic imaging into clinical practice. Such technology has potential to address the needs of diverse populations and reduce health disparities by providing all patients with access to accurate diagnosis and management of skin disease.
Shmuylovich completed his MD/PhD training at the School of Medicine in 2015, earning his doctorate in physics in the laboratory of Sándor Kovács, MD, PhD, a professor of medicine. He then completed a fellowship in pediatric dermatology at the School of Medicine and a residency in dermatology at Barnes-Jewish Hospital before joining the laboratory of Samuel I. Achilefu, PhD, the Michel M. Ter-Pogossian Professor of Radiology, as a postdoctoral researcher.
While an MD/PhD student, Shmuylovich co-founded the education technology company Virtual Nerd, an online alternative to one-on-one math tutoring for high school students. He served as vice president and so-called “Chief Science Nerd” for the company until it was acquired by Pearson in 2013.







