New treatment options for kidney cancer
Researchers at Washington University are making advances in treating kidney cancer patients
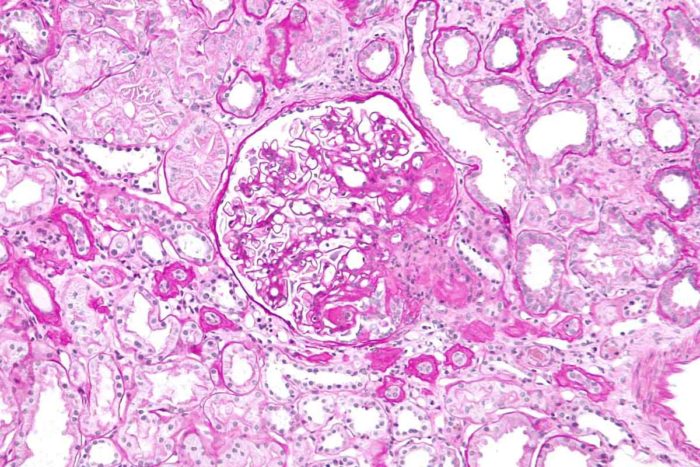
Kidney biopsy. Image courtesy of Wikimedia Commons.
Only decades ago, most kidney cancer patients presented with symptoms—blood in the urine, a mass—and received a diagnosis of advanced disease. Afterwards, they found little in the medical arsenal to help them. Surgery meant a total kidney removal; medical oncology had few cancer drugs to offer. Since studies had shown that patients faced a worse survival rate if they had radiation therapy before or after surgery, its use was limited to use in controlling metastatic disease.
Today, that bleak picture has changed. Thanks to CT and MRI scans, more than 80 percent of kidney cancers are detected incidentally when patients have scans for unrelated reasons. Thus, many tumors are still small, up to four centimeters in size. And exciting treatment options are now available—partial nephrectomy and robotic surgery, new oncology drugs and stereotactic body radiation therapy—some of them developed or refined by physicians and scientists at the Alvin J. Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine.
Surgical innovations
In 90 percent of cases when the tumor is four centimeters or less in size, surgeons at Siteman can perform surgery known as a partial nephrectomy to remove the tumor and save the rest of the kidney, with exactly the same odds of a successful outcome as from a complete nephrectomy. Further, the patient still has at least a kidney and a half remaining, so there is less chance in the long term of renal failure.
In 2007, Sam Bhayani, MD, Washington University urological surgeon at Barnes-Jewish Hospital, developed a successful technique for doing partial nephrectomies robotically. Since then, he has performed this kidney-sparing procedure on five continents; he and his surgical colleague Sherburne Figenshau, MD, have taught it to surgeons internationally. Altogether, nine surgeons in the Division of Urology operate on 500 kidney cancers a year—one of the highest volumes in the world.
“Our first goal is to cure the cancer, and the second is to save the kidney. Achieving those two goals is a home run,” says Bhayani. “If you can do all this robotically with two or three tiny incisions, that’s where quality of life comes in— and it’s not just a home run, it’s a grand slam.”
For patients who are not good operative candidates, Bhayani and his colleagues collaborate with radiologists to perform cryosurgery of the kidney. Inserting one or two needles into the kidney, cryosurgery freezes and kills tiny tumors from one-to-two centimeters in size, thus treating—and most often curing—sicker patients non-operatively.
These leading-edge techniques are the latest advances in a program with a history of innovation. In 1990, Washington University surgeon Ralph Clayman, MD, performed the first laparoscopic total kidney removal in the world at Barnes-Jewish Hospital. His successors are still expert at whole nephrectomy. “If a patient needs a kidney removal, no one has been doing it longer than we have,” says Bhayani.
Medical oncology advances
After a total nephrectomy, the expertise of medical oncologists comes into play, and the range of therapies available to them has changed dramatically in the recent years. Today, oncologists rely on targeted therapies with seven drugs that have lately received approval. Although these drugs carry the risk of toxicity, some patients stay on first-line therapy for up to two years.
“After two decades of no new approvals by the FDA, the picture today is much brighter,” says Bruce Roth, MD, professor of medicine. “While these are not curative therapies in a metastatic setting, we can alter the natural history of the disease and have stabilization or shrinkage, sometimes for a long time. Our goal is to convert this into a chronic disease.”
There are also new clinical trials available, including one that is now recruiting patients. Surgeons remove the patient’s kidney, and then physicians generate a vaccine from that tumor and give it back to the patient with standard therapy. “It is the ultimate in precision medicine,” says Roth.
A new role for radiation therapy
Radiation therapy spent years “on the back burner” as a useful treatment for kidney cancer, says Jeff Michalski, MD, the Carlos Perez Distinguished Professor of Radiation Oncology and vice chair of the Department of Radiation Oncology. “But new techniques today are making us reexamine the role of radiation therapy in small kidney cancers.”
Barnes-Jewish is one of the few hospitals in the United States using stereotactic body radiation therapy to treat early-stage primary kidney cancers, as well as liver, prostate and lung cancers. In this therapy, physicians deliver doses precisely to a small area, combining that therapy.
Currently, they are beginning to use stereotactic body radiation in medically inoperable patients who are not amenable to cryosurgery. While this treatment is still in its investigational stage, the outcome looks promising. If it proves successful, it will open the door to yet another therapeutic approach for these small cancers.







