New inpatient towers cater to women, infants, cancer patients
Buildings designed to enhance patient care, comfort
Huy MachTwo newly opened, 12-story towers on the Washington University Medical Campus enhance patient care and comfort. One of the buildings is the Barnes-Jewish Parkview Tower, which offers facilities for patients of Siteman Cancer Center and the Women & Infants Center. The latter includes a labor and delivery floor that connects via a skywalk to the neonatal intensive care unit (NICU) in the new St. Louis Children’s tower.
The first moments of life for critically ill infants born at Barnes-Jewish Hospital entail an urgent transport from the labor and delivery room to the neonatal intensive care unit (NICU) at St. Louis Children’s Hospital. But soon, due to the newly finished high-rises on the Washington University Medical Campus, the commute will be reduced to seconds.
The two meticulously designed 12-story towers — built by BJC HealthCare — feature floor plans that foster a warm and comfortable environment that will enhance care for women, infants and cancer patients. The buildings’ details — from the hallways and patient rooms to the waiting areas and rooftop gardens — are intentional and designed with input from physicians, caregivers, families and patients.
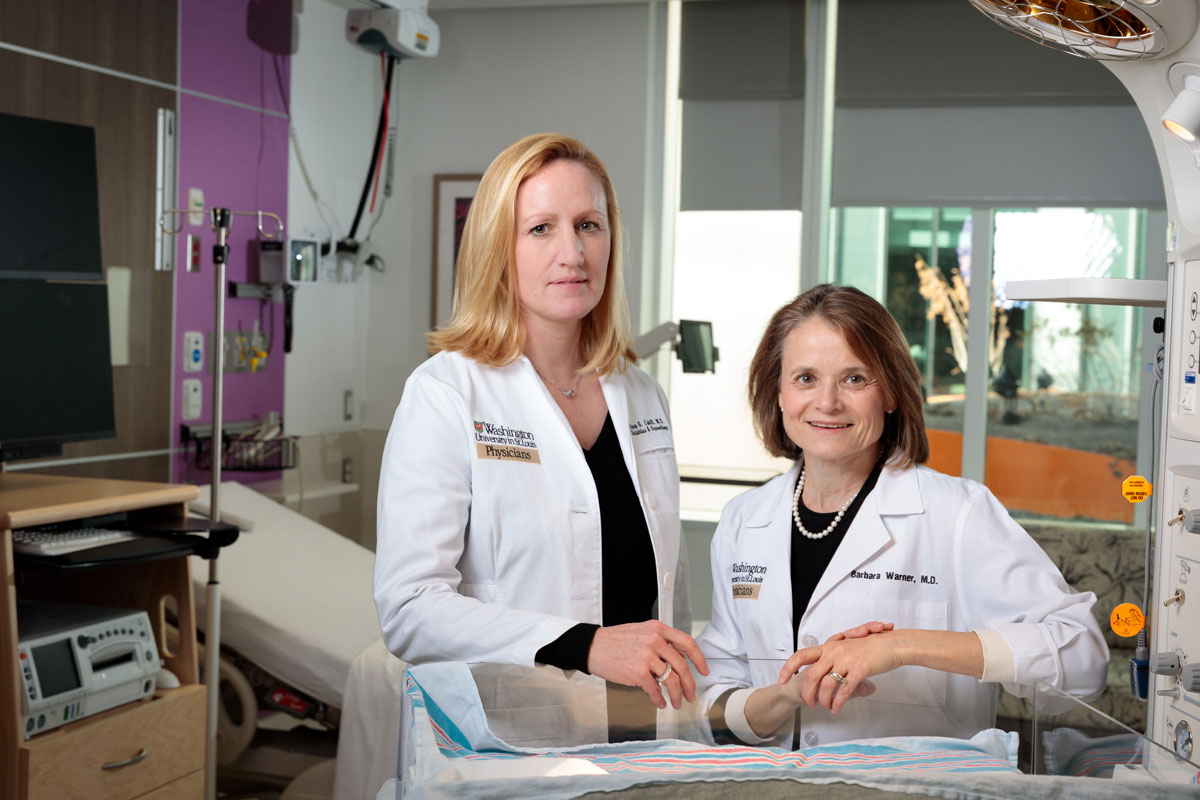
“For patients and their families, and for those of us who care for them, the new facility is game-changing in the best possible way,” said Barbara B. Warner, MD, a professor of pediatrics who cares for infants in the NICU. “The design helps us to be more immediate, efficient and able to provide the best care possible. It also offers calmness and comfort for women, infants and their families, allowing them to focus on their monumental life changes.”
One of the inpatient buildings is the Barnes-Jewish Parkview Tower, which offers roomy and modernized facilities for patients of Siteman Cancer Center and the Women & Infants Center. The latter includes a labor and delivery floor that connects via a skywalk to the NICU in the St. Louis Children’s tower.
The Children’s tower also adds 96 private patient rooms on six floors, addressing the need for more beds for pediatric patients.
Nearly 800 health-care workers, patients and family caregivers strategized with the design team about their specific needs, such as equipment placement, optimal light exposure, color palettes and outlet placement for charging smartphones, laptops and other devices. Spaces feature sleeping accommodations for family and increased storage for personal items. Many rooms also offer views of Forest Park and new rooftop gardens.
The design also recognizes the medical center’s expertise in treating high-risk pregnancies, with a designated state-of-the-art operating room for the most complex fetal surgeries and deliveries, including births of twins, triplets and other multiples. Two other operating rooms cater to women delivering by cesarean section.
Additionally, dedicated patient corridors in the buildings separate foot traffic, helping to increase efficiency among health-care workers while reducing distractions and noise that can interfere with rest and recuperation.
“Our patients are at the heart of these facilities,” said Paul J. Scheel Jr., MD, associate vice chancellor for clinical affairs at the School of Medicine and CEO of Washington University Physicians. “We considered every detail, with the important goal of maximizing patient comfort and care. We wanted a calming, highly functional environment to minimize distractions and stress so the focus always is on improving patient health.”
Women and infants
Fostering the infant-parent bond motivated the design of the new center, which, in addition to labor and delivery, includes 34 private postpartum inpatient beds in wide rooms with sleeper sofas for family. Near each room’s entrance are drawers fully stocked with supplies for diapering and feeding. Retractable curtains and rolling bassinets offer privacy and encourage mother-baby bonding.
“The setup is conducive to breastfeeding and hands-on infant care,” Warner said. “The skywalk connecting labor and delivery with the NICU also gives critically ill infants the best conditions for improved health.”
 Matt Miller
Matt MillerPreviously, it could take almost 10 minutes to transfer critically ill infants to the current NICU at St. Louis Children’s from Barnes-Jewish. “Now, the distance is about 25 yards from labor and delivery to the new NICU,” said Alison Cahill, MD, an associate professor of obstetrics and gynecology and director of the Division of Maternal-Fetal Medicine. “No time is wasted in caring for mothers and babies. Every second counts in life-saving situations.”
Such efficiency is expected to result in less time moving or getting to patients, which will translate into more time for patient care. “The rooms are designed to bring exceptional medicine to patients, from the healthiest to the sickest,” Cahill said.
The expansion of the Children’s Hospital NICU adds 40 beds, bringing the total to 125 beds, most in private rooms. The addition also adds space for pediatric intensive care beds.
Cancer patients
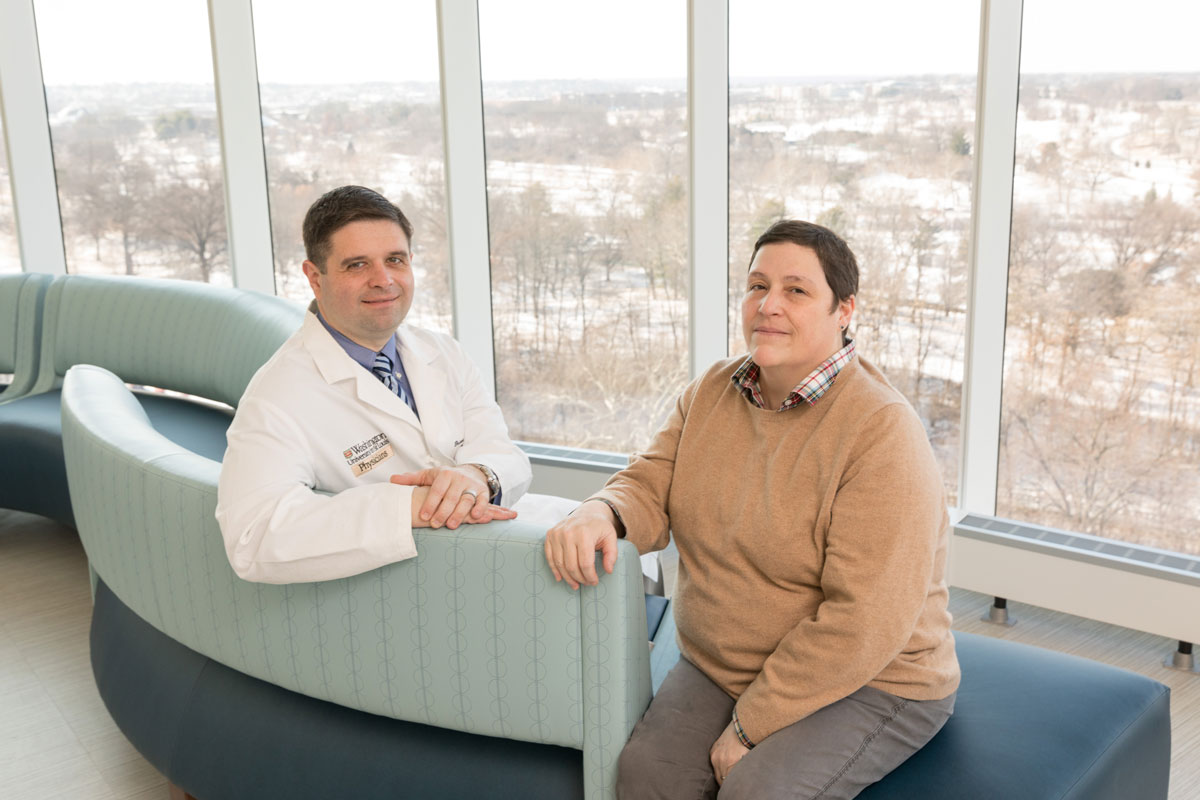
During her year-long treatments for non-Hodgkin lymphoma, a cancer of the immune system, Cindy Fogal formed close relationships with many of her caregivers at Siteman Cancer Center.
She endured nine-hour chemotherapy treatments and extended overnight stays following a stem-cell transplant. “I’d share long stretches of hours, even days, for months on end with particular nurses, during an emotionally and physically fragile time,” said Fogal, who is now in full remission after her cancer diagnosis in 2010. “We became friends.”
Fogal’s concern for her caregivers, coupled with gratitude for the amazing care she received, inspired her to join Siteman’s Patient Family Advisory Council in 2012. The group met with the design team to incorporate patients’ and caregivers’ needs in the Parkview Tower design.
“One of our biggest concerns was how best to care for the caregivers,” Fogal said. “Their job is emotionally taxing, and I felt, as did other patients, that there needed to be a quiet, designated space for the medical staff to reflect and regroup. Tending to their emotional health is not only humane, but it leads to better experiences for patients and their families.”
 Matt Miller
Matt MillerIn the new Parkview Tower, each floor has a dedicated quiet room for health-care workers. Additionally, thanks partly to input from the Patient Family Advisory Council, patient and family waiting areas provide private spaces. “Dealing with cancer is not easy for anyone,” said Fogal, PhD, whose volunteer work at Siteman inspired her to become a clinical research supervisor in oncology at the School of Medicine after having spent years as a senior scientist and microbiology lab instructor in the biology department on the Danforth Campus.
“Many cancer patients also work through their treatments and need a quiet space to do so during downtime at the hospital,” Fogal added. “All of this contributes to fewer stressors, and that benefits everyone.”
The Parkview Tower includes 160 private rooms and 10 bone marrow transplant intensive care unit beds for inpatient care.
“The new facility is incredible, thanks to extensive input from patients, family, physicians, nurses and staff,” said Brian A. Van Tine, MD, PhD, an associate professor of medical oncology. “We can provide the best possible care in this setting. It is a huge asset for the Washington University Medical Campus.”
















