New guidance developed for children hospitalized with mild head trauma
Risk score determines whether kids with abnormal CT scans require ICU care
 Thinkstock
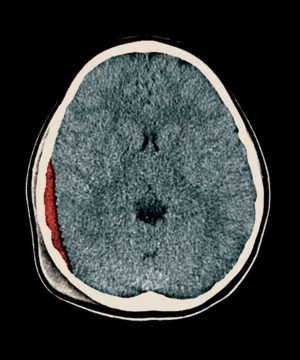
ThinkstockPediatric neurosurgeons at Washington University School of Medicine in St. Louis have developed a new risk scoring system to help standardize care for children with mild traumatic brain injuries who have abnormal CT scans. Such children are at risk of neurological decline. Depending on the details of the CT scan, some can be cared for safely in a general hospital ward, but others require the more intense monitoring of an ICU.
When a child suffers a mild head injury, doctors have well-established protocols for determining whether that child should have a computed tomography (CT) scan to assess the damage. Most children with mild traumatic brain injury have normal CT scans — a scenario often referred to as a concussion.
If a CT scan is abnormal, however, a child’s condition is at higher risk of deteriorating, requiring monitoring in a hospital. But there is little consensus about how closely such children should be monitored. Some such children recover well, while others experience a neurological decline and need surgery to relieve brain swelling.
In new research, pediatric neurosurgeons at Washington University School of Medicine in St. Louis developed a risk scoring system intended to help determine whether a child with mild traumatic brain injury and an abnormal CT scan can be monitored safely in a general hospital ward or requires the increased surveillance of an intensive care unit (ICU).
The study is published Feb. 13 in JAMA Pediatrics.
“We want to care for these children in the safest way possible and at the same time not place kids unnecessarily in ICUs if they don’t need that level of care,” said senior author David D. Limbrick, MD, PhD, a professor of neurological surgery and of pediatrics and director of the Division of Pediatric Neurosurgery. “We have identified factors that indicate which of these patients are likely to experience neurological decline and require surgery and which are not. This information can help health-care providers decide where to place these children when they are admitted into the hospital.”
The researchers plumbed data from more than 40,000 children evaluated from 2004 to 2006 at 25 North American hospital emergency departments, including St. Louis Children’s Hospital.
The information originally was gathered in a study conducted by the Pediatric Emergency Care Applied Research Network (PECARN), which established the standard framework for deciding whether a child with a mild head injury should have a head CT scan. Limbrick and his colleagues returned to this data set for guidance on how to handle the subset of children who receive CT scans and are shown to have abnormal findings on the scans. Of the 40,000 children enrolled in the study, 15,000 had CT scans following mild traumatic brain injury. Of these, 839 patients showed abnormalities on the CT scan, such as a brain bleed.
These types of injuries are serious enough that some children will experience a neurological decline and need surgery to relieve swelling or pressure on the brain.
In the United States, traumatic brain injury leads to almost 600,000 emergency room visits annually. Of new pediatric brain injury cases, more than 90 percent are determined to be mild. About one-third of the 50,000 to 60,000 children hospitalized each year due to head trauma have mild traumatic brain injury.
Based on an analysis of the injuries these patients suffered and how they recovered, the investigators developed a risk score ranging from zero to 24 points, called the Children’s Intracranial Injury Decision Aid score (CHIIDA). Higher scores indicate the patient is at higher risk of neurological decline and should receive increased monitoring. Lower scores mean a patient is at lower risk of neurological decline. A score of zero indicates the child is at very low risk. The chance that such a child would go on to experience a neurological decline that requires surgery is less than 1.5 percent, according to the analysis.
As a general rule, the authors suggested, children with scores of less than three points can safely be admitted to a general ward. Patients with higher scores should receive increased surveillance up to and including that provided in an ICU.
“There is a lot of variability in how these patients are managed,” said first author Jacob K. Greenberg, MD, a resident in neurosurgery at Washington University School of Medicine and St. Louis Children’s Hospital. “When we looked back at the data, we saw situations where children were perhaps put in the ICU but didn’t need to be there. And conversely, some patients were placed in a general ward when their risk factors suggested they needed closer monitoring. We are trying to develop this evidence-based tool to help guide and standardize this decision-making process.”
The score is determined by four factors that the researchers found most predictive of patient outcomes. One factor is called the Glasgow Coma Scale (GCS), which is used to measure how alert and responsive a patient is after a blow to the head. Fifteen is the highest and best GCS score, meaning the patient can open his or her eyes spontaneously, follow commands to move different body parts and answer questions clearly and appropriately.
 St. Louis Children's Hospital
St. Louis Children's HospitalWhile the GCS is based on a doctor’s interaction with a patient, the other three factors are determined based on an analysis of a CT scan. The biggest risk factors seen in a CT image are a depressed skull fracture and what is referred to as a midline shift, when the symmetrical structures of the brain are pushed off-center. The final risk factor is an epidural hematoma — a blood clot between the outer layer of the brain’s protective covering and the inside of the skull.
Patients with mild traumatic brain injury who show these features on a CT scan and also have a lower GCS score are at high risk of experiencing a neurological decline and, according to the researchers, should be cared for in an ICU.
“There are a variety of potential harms associated with sending a patient to an inappropriate location,” Greenberg said. “I think the most important is that if you send a child who needs the ICU into a general hospital ward, you risk missing a potential decline that could have been caught earlier. If the patient experiences new weakness or worsening mental status, for example, the goal is to intervene as quickly as possible to avoid permanent disability or even death.
“On the other hand, if you send too many patients to the ICU, there are significant financial costs there, as well as emotional costs for the family,” he said. “Another concern is the limited space available in pediatric ICUs. Having children in the ICU who don’t need to be there is taking beds away from other patients who do need those resources.”







