Nerve injury appears to be root of diabetes-related vision loss
Treatment early in disease may help patients with diabetic retinopathy
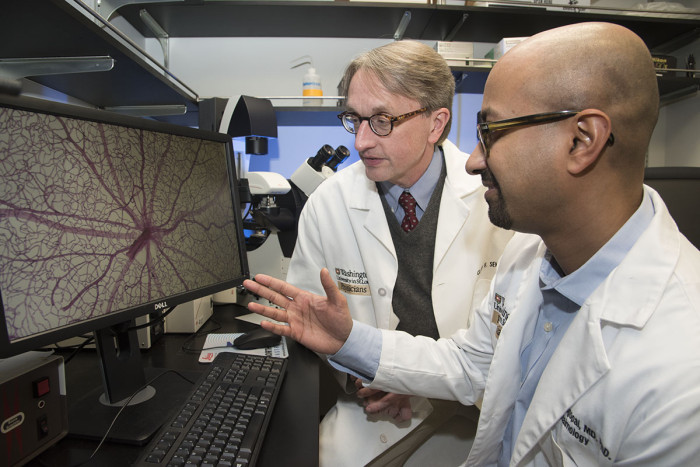 Robert Boston
Robert BostonRithwick Rajagopal, MD, PhD (foreground), and Clay F. Semenkovich, MD, view an image of a mouse retina damaged by diabetes. They found that nerve damage in the retina precedes the development of abnormal blood vessels normally blamed for vision loss in diabetic retinopathy.

Diabetes-related vision loss most often is blamed on blood vessel damage in and around the retina, but new research indicates that much of that vision loss may result from nerve cell injury that occurs long before any blood vessels are damaged.
The finding — from scientists at Washington University School of Medicine in St. Louis — may lead to new approaches to treating diabetes-related vision loss, called diabetic retinopathy, since many current treatments are aimed at damaged blood vessels.
“Many of my colleagues believe if you catch diabetic retinopathy early enough, it can be controlled with drugs that combat damage to blood vessels,” said first author and ophthalmologist Rithwick Rajagopal, MD, PhD. “But those drugs have side effects, and the drugs are very expensive. In addition, our findings suggest there is an underlying, progressive neurodegeneration not being addressed by those therapies.”
The study is published in the April issue of the journal Diabetes.
The obesity epidemic has sparked a diabetes epidemic. Some 30 million people in the U.S. have some form of diabetes. As the number of people with diabetes has increased, so has the number of those with diabetic retinopathy, now the most common cause of new cases of blindness worldwide in adults ages 20-74.
Working in the laboratory of Clay F. Semenkovich, MD, the Irene E. and Michael M. Karl Professor and chief of the Division of Endocrinology, Metabolism & Lipid Research, Rajagopal fed mice a high-fat diet to induce diabetes and, eventually, diabetic retinopathy. When researchers tested animals after two and then three months, they couldn’t find any problems in the mice’s eyes.
But after three months on the high-fat diet, the animals had developed obesity-related glucose intolerance, and by six months, they had nerve problems in the retina. There was no evidence of blood vessel damage in the eyes, however, until the animals were examined at 12 months.
“Interestingly, the disease came on so slowly that we were able to identify different stages of the disease,” Rajagopal said. “We found that they developed functional problems in the retina from nerve cell defects much earlier than they developed the vascular disease we normally associate with mouse and human retinopathy.”
Although current treatments for diabetic retinopathy help many people, the benefit might be greater if patients received therapies earlier in the course of the disease, particularly treatments focused on treating nerve damage, said Semenkovich, who also is a professor of cell biology and physiology.
“There is evidence from other studies that people with diabetes go through a phase that seems to correspond to the early nerve injury we found in the retinas of these mice,” he said. “But that has been largely overlooked by many in the field because the dogma has it that diabetic retinopathy is a disease of the blood vessels.”
The most profound implication of the study is that injury to nerve tissue in the retina may occur much earlier than damage to blood vessels in the eye, Semenkovich explained.
“Now we have an animal model that may help us develop therapies that address nerve damage that appears to occur long before blood vessel damage begins,” he said.







