Nanoparticle injections may be future of osteoarthritis treatment
Mouse study shows particles may reduce inflammation, stop destruction of cartilage
 Pham laboratory
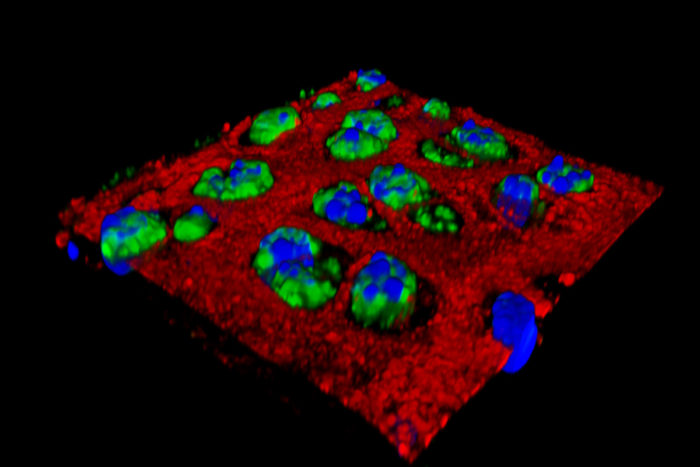
Pham laboratoryResearchers at Washington University School of Medicine in St. Louis have found that injecting nanoparticles into an injured joint can inhibit the inflammation that contributes to the cartilage damage seen in osteoarthritis. Shown in green is an inflammatory protein in cartilage cells. After nanoparticles are injected, the inflammation is greatly reduced.

Osteoarthritis is a debilitating condition that affects at least 27 million people in the United States, and at least 12 percent of osteoarthritis cases stem from earlier injuries. Over-the-counter painkillers, such as anti-inflammatory drugs, help reduce pain but do not stop unrelenting cartilage destruction. Consequently, pain related to the condition only gets worse.
Now, researchers at Washington University School of Medicine in St. Louis have shown in mice that they can inject nanoparticles into an injured joint and suppress inflammation immediately following an injury, reducing the destruction of cartilage.
The findings are reported online Sept. 26 in the early edition of the Proceedings of the National Academy of Sciences.
“I see a lot of patients with osteoarthritis, and there’s really no treatment,” said senior author Christine Pham, MD, an associate professor of medicine. “We try to treat their symptoms, but even when we inject steroids into an arthritic joint, the drug only remains for up to a few hours, and then it’s cleared. These nanoparticles remain in the joint longer and help prevent cartilage degeneration.”
Frequently, an osteoarthritis patient has suffered an earlier injury — a torn meniscus or ACL injury in the knee, a fall, car accident or other trauma. The body naturally responds to such injuries in the joints with robust inflammation. Patients typically take drugs such as acetaminophen and ibuprofen, and as pain gets worse, injections of steroids also can provide pain relief, but their effects are short-lived.
In this study, the nanoparticles were injected shortly after an injury, and within 24 hours, the nanoparticles were at work taming inflammation in the joint. But unlike steroid injections that are quickly cleared, the particles remained in cartilage cells in the joints for weeks.
The nanoparticles used in the study are more than 10 times smaller than a red blood cell, which helps them penetrate deeply into tissues. The particles carry a peptide derived from a natural protein called melittin that has been modified to enable it to bind to a molecule called small interfering RNA (siRNA). The melittin delivers siRNA to the damaged joint, interfering with inflammation in cells.
The peptide-based nanoparticle was designed by study co-investigators Hua Pan, PhD, an assistant professor of medicine, and Samuel Wickline, MD, the James R. Hornsby Family Professor of Biomedical Sciences.
“The nanoparticles are injected directly into the joint, and due to their size, they easily penetrate into the cartilage to enter the injured cells,” Wickline said. “Previously, we’ve delivered nanoparticles through the bloodstream and shown that they inhibit inflammation in a model of rheumatoid arthritis. In this study, they were injected locally into the joint and given a chance to penetrate into the injured cartilage.”
The nanoparticles were injected shortly after injury to prevent the cartilage breakdown that eventually leads to osteoarthritis. Whether such a strategy will work years after an injury, when osteoarthritis is established and there is severe cartilage loss, still needs to be studied. But the findings suggest that the nanoparticles, if given soon after joint injuries occur, could help maintain cartilage viability and prevent the progression to osteoarthritis.
“The inflammatory molecule that we’re targeting not only causes problems after an injury, but it’s also responsible for a great deal of inflammation in advanced cases of osteoarthritis,” said Linda J. Sandell, PhD, the Mildred B. Simon Research Professor of Orthopaedic Surgery and director of Washington University’s Center for Musculoskeletal Research. “So we think these nanoparticles may be helpful in patients who already have arthritis, and we’re working to develop experiments to test that idea.”







