Lung transplantation: Bench science pursues solutions for long-term survival
Research at Washington University School of Medicine is helping to improve the survival of patients who receive lung transplants
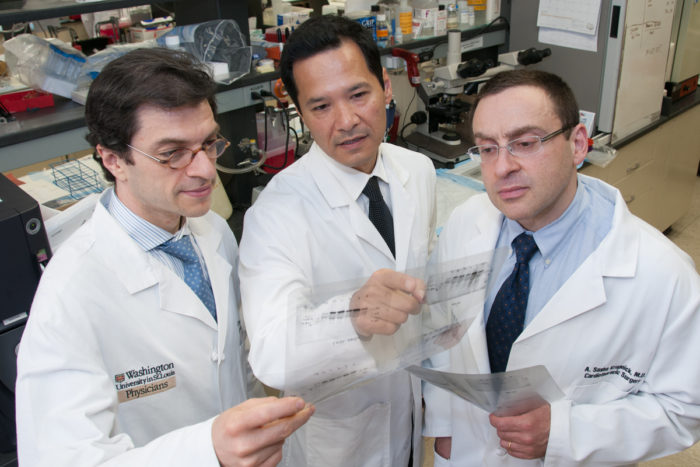
From left, Daniel Kreisel, MD, PhD, Andrew Gelman, PhD, Alexander Krupnick, MD, have established a large combined laboratory to investigate lung immunology and transplantation.
Because of the lung’s unique characteristics, the success of lung transplantation lags behind other solid organs. Lung transplant specialists at Washington University School of Medicine and Barnes-Jewish Hospital are optimizing treatment for lung transplant recipients, and their ongoing research may hold the key to understanding why rejection sometimes occurs and is offering recipients hope so that they may lead longer and better lives.
“The lung is itself an immune organ,” says lung transplant surgeon G. Alexander Patterson, MD. “It’s full of tissues, lymph nodes and inflammatory cells, and it’s in constant contact with the outside environment.” This is one reason why lung transplant recipients often need more immune suppression than patients who receive hearts or kidneys or livers, he adds.
Care guidelines evolve
Patterson, one of the surgeons who performed the world’s first successful lung transplant at the University of Toronto in 1983, has seen lung transplant patients benefit from international guidelines and standardization of surgical techniques, immunosuppression and donor/recipient selection. Barnes-Jewish Hospital is one of the highest-volume centers in the United States with 55-60 lung transplants a year; Patterson attributes the program’s success to each team member’s expertise and the preference for bilateral, or double-lung transplant, which results in better outcomes than single-lung transplant.
The dual risks of lung transplant are rejection and infections, which pulmonologists must balance through the immunosuppressive regimen.
When Barnes-Jewish Hospital became one of the earliest U.S. lung transplant centers in 1988, the standard regimen was to use immune suppression drugs such as cyclosporine, azathioprine and prednisone. After newer drugs such as tacrolimus and mycophenolic acid were introduced in the mid-1990s, the prevalence of treated organ transplant, or graft rejection in the first year dropped from about 50 percent to 25 percent today for all transplants.
“Whether that is cause and effect, I don’t think anybody knows,” says pulmonologist Elbert Trulock III, MD.
In the past 10 years, Washington University pulmonologists at Barnes-Jewish Hospital have used a special drug regimen to treat patients who have HLA antibodies, which are associated with chronic rejection. To slow the decline of lung function in patients with additional causes of chronic rejection, the physicians also use extracorporeal photophoresis (ECP), which removes and treats white blood cells before returning them to the bloodstream. Although ECP has not been tested extensively, “anecdotally it’s probably the best treatment there is for chronic rejection,” says Ramsey Hachem, MD, medical director of the lung transplant program.
New clues from the laboratory
Despite advancements in treatment and early survival, increasing long-term survival has remained elusive. Five years after transplantation, fewer than half of transplanted lungs are still functioning, according to the U.S. Organ Procurement and Transplantation Network. In comparison, the survival rates for heart, kidney and liver transplants are about 70 percent.
Lung transplant surgeons Daniel Kreisel, MD, PhD, and Alexander Krupnick, MD, and transplant immunologist Andrew Gelman, PhD, developed a mouse model of lung transplantation in 2007 to better understand cellular and molecular mechanisms contributing to lung graft injury. In February 2014, they published a report that newly transplanted lungs in mice were more likely to be rejected if key immune cells—memory T cells—were missing, a situation that simulates what happens when patients take certain immunosuppressive drugs.
“A lot of transplant recipients receive drugs that indiscriminately deplete many different T cells,” says Kreisel. “But in lung transplants, this strategy may contribute to organ rejection.”
Kreisel, Krupnick and Gelman next will look for ways to encourage memory T cells to thrive while eliminating other T cells that harm transplanted lungs. A possible platform for this is an ex vivo lung perfusion system, where the lungs are treated with a solution outside of the body to improve their quality before transplantation. This system is currently being tested at Washington University for another purpose—to evaluate marginal lungs for human transplants—but could be adapted to the mouse model.
“Our goal is to eventually establish a personalized method to achieve graft tolerance using ex vivo perfusion,” says Krupnick. They plan to harvest T cells from potential recipients. They would then use these cells to condition the lung graft using the ex vivo perfusion system prior to transplanting the graft.
Research focusing on these early events may ultimately be able to boost late survival.







