Like Zika, West Nile virus causes fetal brain damage, death in mice
Viruses related to Zika may share its ability to harm fetuses
 Nitin Arora
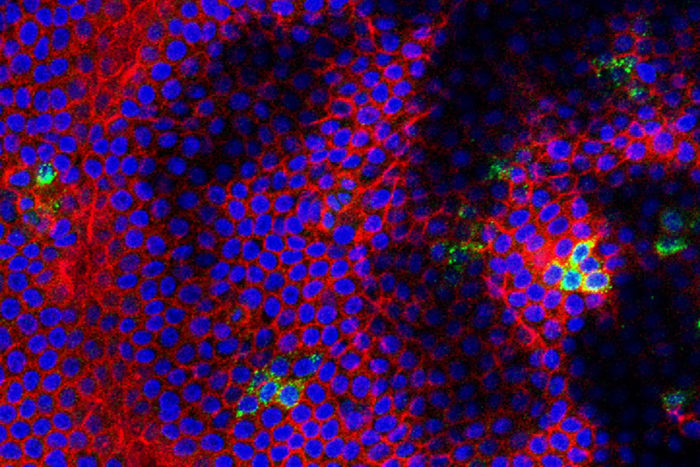
Nitin AroraWest Nile virus (green) grows in human placenta, where the cells are marked red with blue nuclei. A study has found that viruses related to Zika, such as West Nile, can cross the placenta in mice and cause fetal brain damage and death.
Two viruses closely related to Zika – West Nile and Powassan – can spread from an infected pregnant mouse to her fetuses, causing brain damage and fetal death, according to a new study from Washington University School of Medicine in St. Louis. The findings suggest that Zika may not be unique in its ability to cause miscarriages and birth defects.
“We only studied mice and human tissues, so we can’t say for sure what happens when pregnant women are infected with these viruses,” said Jonathan Miner, MD, PhD, an assistant professor of medicine and the study’s senior author. “But our findings suggest that it is possible that viruses related to Zika, such as West Nile, pose the same risk to developing fetuses that Zika does.”
The study is published Jan. 31 in Science Translational Medicine.
Zika virus garnered worldwide attention beginning in 2015, when reports of an outbreak surfaced in Brazil. Alarm heightened when researchers linked Zika infection in pregnant women with the risk of bearing babies born with microcephaly, or abnormally small heads.
Miner, who helped develop mouse models of Zika virus infection during pregnancy while working in the laboratory of Michael Diamond, MD, PhD, stumbled across a few scattered reports in medical literature suggesting that West Nile virus also could be spread from mother to child before birth, causing birth defects. But nobody had rigorously tested the possibility by comparing multiple viruses in parallel.
Miner and graduate student Derek Platt, the study’s first author, decided to find out whether West Nile and a related virus known as Powassan could cause similar brain damage and fetal death. Like Zika, both belong to the flavivirus family and target neural tissues.
West Nile infects thousands of people every year in the United States. Most never know they have it, but about 1,000 people a year develop life-threatening brain infections that can cause persistent neurological problems.
Powassan is a rare virus spread by ticks. There are only a few dozen documented cases of disease caused by the virus in the U.S. over the past decade, mostly in the Great Lakes region.
As part of the study and for comparison, Platt and Miner also wanted to study the effects of two mosquito-borne viruses only distantly related to Zika: chikungunya and Mayaro. Both are found in Brazil and can cause arthritis.
They injected female mice at day six of their pregnancies with one of the four viruses, then examined the placentas and fetuses a week later.
All four viruses infected the placentas and fetuses, but levels of West Nile virus were 23- to 1,500-fold higher than those of the other three viruses in the placentas, and 3,000- to 16,000-fold higher in the heads of the fetal mice.
In addition, brain tissue from West Nile-infected fetuses showed severe damage under the microscope, while brain tissue from chikungunya-infected fetuses appeared healthy.
Miner and Platt also found that about half of the fetuses whose mothers were infected with West Nile or Powassan virus died within 12 days of infection, whereas no fetuses from mothers infected with chikungunya or Mayaro died.
With the help of Diamond and Carolyn Coyne, PhD, of the University of Pittsburgh, the researchers then infected human placentas with one of the four viruses or Zika virus. They found that the three flaviviruses – Zika, West Nile and Powassan – multiplied in human placentas while chikungunya and Mayaro did not.
“Millions of people were infected with Zika in a short time, and I think that made it easier to see, in people, that Zika virus could infect and cross the placenta and cause fetal damage,” said Miner, who is also an assistant professor of molecular microbiology and of pathology and immunology. “But our data show that other flaviviruses have the same capacity, at least in mice. It may be that it’s just more difficult to prove a link between West Nile and birth defects because the number of cases is smaller and infections are more sporadic.”
Additional epidemiologic studies to determine whether West Nile infection can cause miscarriage and brain damage in people may be prompted by this discovery, Miner said.
“I don’t want people to think that we’re saying West Nile is definitely a threat to pregnant women and their babies,” Miner said. “We’re saying it’s possible. But until we know for sure, it’s always a good idea to wear bug repellant.”







