Culprit identified as a major cause of vision loss
Finding may lead to treatments for retinal diseases including retinitis pigmentosa
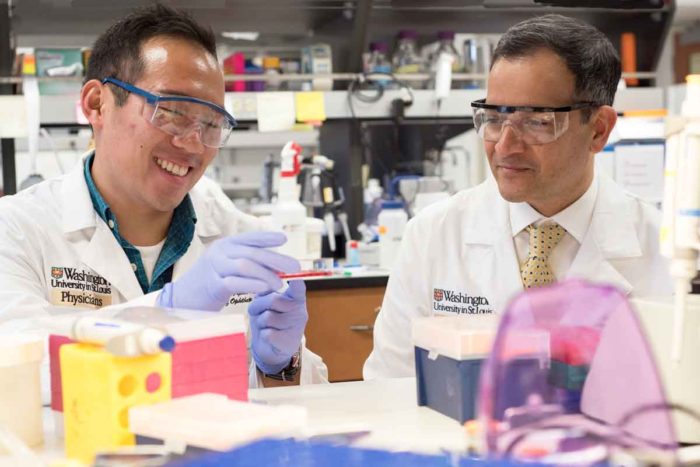 Robert Boston
Robert BostonMD/PhD student Jonathan Lin (left) and Rajendra S. Apte, MD, PhD, of Washington University School of Medicine in St. Louis, have identified a pathway involved in photoreceptor death in the retina. They also have found a way to reverse damage to those cells, potentially providing a treatment strategy for blinding diseases such as retinitis pigmentosa.

The eye’s retina works like film in a camera. The retina’s rods sense dim light, while cone cells detect colors, contrasts and sharp images seen during daylight. A wide range of disorders can damage those rods and cones and lead to vision loss. But now, researchers at Washington University School of Medicine in St. Louis have identified a pathway involved in harming rods and cones and have found a way to halt that damage.
Targeting the pathway with therapies could save sight in patients with many types of retinal disorders, including those for which there are no treatments, such as retinitis pigmentosa and advanced dry age-related macular degeneration.
The findings, from studies in mice and in retinal cells, are published Sept. 27 in the journal Cell Reports.
“We believe we have uncovered a unifying pathway involved in inflicting severe damage to and even causing the death of rods and cones,” said Jonathan B. Lin, an MD/PhD student and co-first author with Shunsuke Kubota, MD, PhD, a former postdoctoral fellow at the School of Medicine. “These findings should help us develop treatments for retinal disorders, regardless of what’s causing them.”
Lin works in the laboratory of senior investigator Rajendra S. Apte, MD, PhD, the Paul A. Cibis Distinguished Professor of Ophthalmology and Visual Sciences. In a series of experiments first in mice and later in retinal cells, they identified a key molecule — NAD — in the cascade that leads to the death of the retina’s rods and cones.
Photoreceptor cells such as rods and cones are among the biggest users of energy in the body. The researchers identified problems in the cells’ mitochondria — the cells’ engines, where energy is produced — as a culprit in vision loss. The NAD molecule is well-known for its important role in energy production. Further, recent research has identified gene mutations along the NAD pathway as having a role in a disease that causes babies to go blind.
As Lin, Apte and colleagues studied several diseases of the retina, they found that defects in the same NAD pathway appeared to be involved in those disorders, too. When they then treated damaged photoreceptor cells in mice with a second molecule called NMN — a precursor molecule that boosts levels of NAD — the cells’ degeneration ceased and vision was restored. NMN is of particular interest to scientists who study problems related to aging.
“Deficiencies in the energy pathway led to problems, including damage to rods and cones and even photoreceptor death,” said Apte, also a professor of developmental biology and neuroscience and of medicine. “This is exciting because we may have found a reason why these highly metabolically active cells are susceptible to damage and death when the NAD pathway does not function optimally.”
The pathway could be a potential target for therapies for multiple retinal diseases. However, Apte is most excited about what it may mean for conditions such as retinitis pigmentosa.
“It’s one of the leading causes of blindness, and it harms vision more slowly than many other retinal diseases, causing vision loss over the course of many years,” Apte said. “That gives us a much larger therapeutic window.”
Because there are no treatments, Apte said there is potential to make a big difference in patients’ quality of life. In addition, since scientists already are experimenting with the NAD pathway — with some even planning to test treatments involving the NMN molecule — Apte expects clinical trials in people could begin soon.







