Overlooked signal in MRI scans reflects amount, kind of brain cells
Data may aid diagnosis of brain conditions, shed light on brain development
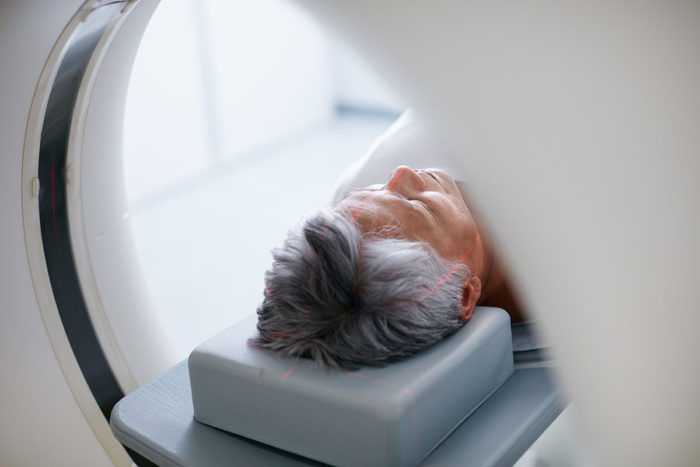 Getty Images
Getty ImagesA six-minute MRI scan gives enough data for researchers to study how the brain develops, or to detect the loss of brain cells due to injury or illness.
An MRI scan often generates an ocean of data, most of which is never used. When overlooked data is analyzed using a new technique developed at Washington University School of Medicine in St. Louis, they surprisingly reveal how many and which brain cells are present – and show where cells have been lost through injury or disease.
The findings, published online the week of Sept. 24 in Proceedings of the National Academy of Sciences, eventually may lead to new ways to diagnose Alzheimer’s disease, multiple sclerosis, traumatic brain injury, autism and other brain conditions through a simple brain scan.
“There’s no easy way to detect the loss of neurons in living people, but such loss plays a role in many neurological diseases,” said Dmitriy Yablonskiy, PhD, a professor of radiology at the university’s Mallinckrodt Institute of Radiology, who directed this study together with Marcus Raichle, MD, a professor of radiology and the Alan A. and Edith L. Wolff Distinguished Professor of Medicine. “We’ve shown in the past that there’s a signal that goes down in parts of the brain in people with Alzheimer’s disease, multiple sclerosis and traumatic brain injury, but we didn’t know what it meant. Now, we know it means neurons have died in those areas.”
Most researchers studying brain function with MRI are only interested in a small portion of the MRI signal. They want to see how the MRI signal changes when a person performs a task, not what stays the same. Researchers trying to understand vision, for example, focus on the signal variation due to the brain activity when a person looks at a picture, and discard the parts of the signal that hold steady. But that is like looking at the waves along the surface of the ocean, and ignoring the mass of water beneath.
Yablonskiy, Raichle and colleagues including Jie Wen, PhD, an instructor in radiology and the study’s first author, Manu Goyal, MD, an assistant professor of radiology and of neurology, and Serguei Astafiev, PhD, a senior scientist in psychiatry, decided to find what the rest of the ocean could tell us about how the brain works.
They analyzed the background data on an MRI scan and found a signal, which they called R2t*, that remained largely unchanged when people performed tasks but varied across parts of the brain. Then, they compared the R2t* signal with data from the Allen Human Brain Atlas, which maps genes active in various areas of the brain. The researchers found three sets of gene networks that tracked with the R2t* signal – the genes were more active where the signal was strong, and less active where the signal was weak. These groups of genes, it turned out, reflected the different kinds and numbers of brain cells, and the extent of connections between them.
In other words, this quick new MRI scan gave the researchers all they needed to know to determine how densely packed and interconnected the neurons are in any part of the brain. This information could help us understand how a person’s brain develops and changes from infancy to old age, and how we build memories and learn. It could also give clues to brain illness or injury.
“We did some studies on traumatic brain injury where we found some areas of the brain are already losing neurons even though the standard scans show nothing,” Yablonskiy said.
The researchers also applied their technique to the hippocampus – the memory center of the brain – in people with Alzheimer’s disease. They found that not only was the hippocampus smaller than in healthy people, but the remaining part was not healthy – it had lost cells and begun to decay.
“There are MRI scans now that can detect brain atrophy even before people show symptoms of Alzheimer’s disease,” Yablonskiy said. “Our technique can show the brain degrading even before it begins to atrophy.”
Yablonskiy and colleagues are now working on applying their technique to brain diseases and disorders including Alzheimer’s, schizophrenia, multiple sclerosis and autism, as well as to understanding how a healthy brain develops and grows.
“We’ve developed a method that takes a six-minute scan and tells you what types of cells are there and how extensively they’re connected,” Yablonskiy said. “As babies develop, neurons start growing, they connect with each other, they start forming memories. Nobody really knows how this is done. But this method could help us understand normal development, as well as how brain diseases develop.”







