AAAS names 7 Washington University faculty as 2020 fellows
Four of the newly named fellows are School of Medicine faculty
 Washington University School of Medicine
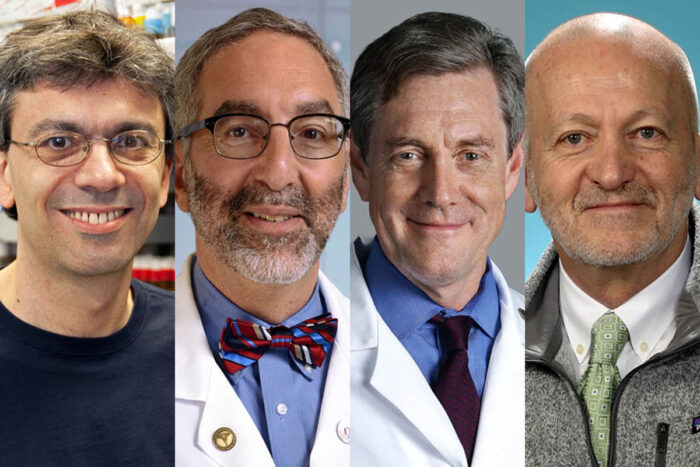
Washington University School of MedicineOf seven faculty members at Washington University selected by the American Association for the Advancement of Science (AAAS) as 2020 fellows, four are at the School of Medicine. They are Aaron DiAntonio, MD, PhD; David H. Gutmann, MD, PhD; Douglas L. Mann, MD; and Paul H. Taghert, PhD. The others, on the Danforth Campus, are John Baugh, PhD; Barbara Kunkel, PhD; and Lan Yang, PhD.
Seven faculty members at Washington University in St. Louis are among 489 new fellows selected by the American Association for the Advancement of Science (AAAS), the world’s largest general scientific society. And four of those seven are School of Medicine faculty.
The newly selected fellows from the medical school are: Aaron DiAntonio, MD, PhD; David H. Gutmann, MD, PhD; Douglas L. Mann, MD; and Paul H. Taghert, PhD. The others, on the Danforth Campus, are John Baugh, PhD; Barbara Kunkel, PhD; and Lan Yang, PhD. Each will receive the highest honor awarded by AAAS in recognition of distinguished efforts to advance science or its applications.
The seven new fellows will be formally announced in the Nov. 27 issue of the journal Science and inducted Feb. 13 during the 2021 AAAS Annual Meeting, to be held online.
Here are details on the School of Medicine’s four new fellows:
David H. Gutmann
Gutmann, the Donald O. Schnuck Family Professor and vice chair for research affairs in the Department of Neurology, is being honored for distinguished contributions to the field of human neurogenetics. His work has helped define the cellular and molecular causes of neurofibromatosis (NF) and related disorders.
Gutmann has dedicated his academic career to understanding NF, complex genetic disorders that cause tumors to grow on nerves in the brain and throughout the body. He founded and directs the Washington University NF Center, one of the world’s largest centers focused on accelerating the pace of scientific discovery and its application to the care of individuals with NF.
Over the past 25 years, his team identified the cells of origin for these cancers and demonstrated that noncancerous cells, such as neurons, microglia and T cells, control the formation and growth of brain tumors in mice that resemble their human counterparts. He has shown that NF tumor cells release factors that attract immune cells, such as microglia and T cells, to the tumor, and induce these immune cells to nurture, rather than attack, the tumors. Further, he has shown that targeting immune cells slows tumor growth in mice, a finding that opens up new avenues of research into potential therapies for low-grade brain tumors.
In addition, Gutmann and his colleagues have leveraged human stem cells and genetically engineered mice to define the factors that underlie disease risk, with the goal of improving precision medicine for this disease. Their findings could provide new ways to help doctors predict which brain tumors are most likely to lead to vision loss, a common complication of NF brain tumors. His work also opens up new avenues to prevent or treat brain tumors.
Gutmann earned his bachelor’s, master’s, doctoral and medical degrees at the University of Michigan. He completed a medical residency in neurology at the University of Pennsylvania and a research fellowship at Michigan. He joined the faculty at Washington University School of Medicine in 1993.
Aaron DiAntonio
DiAntonio, MD, PhD, the Alan A. and Edith L. Wolff Professor of Developmental Biology, is being honored for distinguished contributions to the field of molecular and cellular neuroscience, particularly for studies of axon injury response pathways and mechanisms of pathological axon degeneration.
DiAntonio’s laboratory studies how connections between nerve cells form, are maintained, and respond to injury or disease. Axons, the electrical wiring of the nervous system, can degenerate following injury or due to various neurological disorders. Loss of axons can be devastating, leading to a wide range of disorders including peripheral neuropathy, traumatic brain injury, and glaucoma. In close collaboration with the lab of Jeffrey Milbrandt, MD, PhD, the James S. McDonnell Professor and head of the Department of Genetics, DiAntonio’s group has uncovered the molecular pathways that trigger axon self-destruction and has discovered how to block this signal and preserve functional connections in the injured and diseased nervous system.
He is a co-founder of Disarm Therapeutics, a company that was created to develop new therapies to treat or prevent axonal degeneration, advancements that could be useful in helping patients with a wide spectrum of neurological diseases and injuries. The company recently was acquired by Eli Lilly.
DiAntonio has received outstanding faculty mentorship awards at Washington University, as well as a Javits Neuroscience Award from the National Institutes of Health (NIH) and faculty development awards from the Keck, McKnight, and Sloan Foundations.
He earned his bachelor’s degree in biochemistry from Harvard University and a master’s degree in biochemistry from Cambridge University. He went on to earn his medical degree and doctorate from Stanford University and continued his training with a postdoctoral fellowship at the University of California at Berkeley. In 1999, he joined the faculty of Washington University School of Medicine in the Department of Developmental Biology, and in 2014, he was named the Alan A. and Edith L. Wolf Professor of Developmental Biology.
Douglas L. Mann
Mann, MD, the Tobias & Hortense Lewin Distinguished Professor of Cardiovascular Disease, is being honored for distinguished contributions to cardiology, particularly for discovering the role of cytokine mediated inflammation in causing heart failure and for suggesting novel therapeutic approaches based on this concept.
Mann’s research team is interested in understanding heart failure on a cellular and molecular level, especially the roles of immune cells in either protecting and healing the heart after injury or in perpetuating a damaging inflammatory response. A key focus is on developing ways to promote healing processes and reduce or stop damaging inflammation. Mann’s basic research in the lab in cellular and mouse models of disease has led to several translational clinical trials. He has served as the principal investigator on phase 3 clinical trials that have investigated methods for reducing inflammation or stopping the damaging changes to the heart muscle in patients with heart failure.
Mann has been recognized with numerous awards for his contributions to cardiovascular research and mentorship, including the distinguished mentor award from the American College of Cardiology, the Hugh McCullough Award from the American Heart Association, the Lifetime Achievement Award from the Heart Failure Society of America, and the Michael DeBakey Excellence in Research Award. He is the founding editor of JACC: Basic to Translational Science. He is a past president of the Heart Failure Society of America.
Mann earned his bachelor’s degree in biology from Lafayette College in Easton, Pa., and his medical degree from Temple University School of Medicine in Philadelphia. After completing an internship and residency at Temple University Hospital, he continued his training at the University of California at San Diego, and then at Massachusetts General Hospital. In 2009, he became director of the Cardiovascular Division at Washington University School of Medicine. He was instrumental in opening the Heart and Vascular Center at Barnes-Jewish Hospital and the School of Medicine.
Paul H. Taghert
Taghert, PhD, a professor and interim head of the Department of Neuroscience, is being honored for distinguished contributions to the field of circadian rhythm neuroscience, including new insights on the role of neuropeptides in neuronal circuits.
Circadian rhythms play a role in many aspects of health and disease. For example, jet lag, shift work and disturbances in sleep-activity cycles all undermine mental and physical well-being. Research into the fruit fly Drosophila laid the foundations for the current understanding of the molecular time-keeping mechanism underlying the 24-hour clock. But it remains unknown how a single primary molecular clock is translated into multiple daily rhythms.
By studying the brains of fruit flies, Taghert and colleagues discovered how the brain translates the circadian signal into discrete phases of neuronal activity. Using genetics and novel imaging techniques to perform brain-wide scanning in real time over an entire day, they showed that different groups of pacemaker neurons become active in a precise sequence over the course of a day. These discrete oscillators set different phases of the circadian cycle and thereby control different physiological functions. Taghert showed that the multiplicity of neuronal phases derives from environmental signals such as sunlight and, importantly, from cellular interactions between pacemakers themselves, including signaling via specific neuropeptides such as PDF. PDF delays the activity periods of different pacemakers to specific phases of the day or night.
Taghert’s lab also identified the receptor for PDF, and his group is working to define the signaling pathways through which it has such long-lasting effects on its target pacemaker groups.
Taghert earned his bachelor’s degree in biology from Reed College and a doctoral degree in zoology from the University of Washington in Seattle. He completed postdoctoral research at Stanford University before joining the faculty at Washington University School of Medicine in 1984.







