$5.1 million aimed at preventing superbugs, infections in health-care settings
Funding is part of $26 million awarded by the CDC to five academic medical centers as part of a patient-safety effort
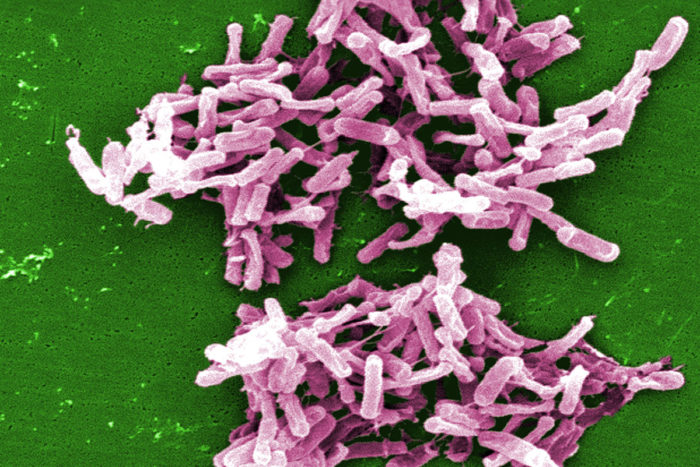 Janice Carr/CDC
Janice Carr/CDCThis micrograph depicts C. difficile bacteria, which can cause severe diarrhea, fever, intestinal pain and, in some cases, death. The infection can occur after prolonged antibiotic use.
Buoyed by a $5.1 million grant, researchers at Washington University School of Medicine in St. Louis will study novel strategies to reduce infections acquired in health-care settings and to limit the spread of dangerous antibiotic-resistant bacteria.
The funding is part of $26 million awarded by the Centers for Disease Control and Prevention (CDC) to five academic medical centers as part of a patient-safety effort known as the Prevention Epicenters Program. Together with the CDC, these Prevention Epicenters develop and test innovative approaches to preventing infections and improving patient safety in health-care settings. The new funding more than doubles previous awards and extends the Prevention Epicenters Program to 2020.
Infections in health-care settings affect more than 700,000 U.S. patients annually and cost nearly $10 billion to treat, according to the CDC. Some of the most serious infections are caused by bacteria that have evolved to become resistant to treatment with antibiotics.
The School of Medicine will collaborate with colleagues at Barnes-Jewish Hospital, St. Louis Children’s Hospital and 11 other BJC HealthCare hospitals and patient-care centers. Together, they form the CDC’s Washington University and BJC Healthcare Prevention Epicenter.
“Health-care-related infections and antibiotic resistance are major public health problems in the U.S. and across the globe,” said Victoria J. Fraser, MD, head of the university’s Department of Medicine and principal investigator of the four-year grant awarded by the CDC to Washington University and its partners.
“There is a gap in knowledge about ways to prevent the overuse of antibiotics — the main cause of patients developing dangerous drug-resistant infections — and a need for more research on innovative strategies to prevent health-care-associated infections,” said Fraser, the Adolphus Busch Professor of Medicine and physician-in-chief at Barnes-Jewish Hospital. “With the CDC’s help, we have made significant improvements in reducing infections in health-care settings and, thereby, reducing the need for antibiotics. But health-care-associated infections and antibiotic resistance remain serious issues, and we still have a long way to go.”
Although health-care-associated infections in the United States have decreased somewhat in recent years, a CDC report published this year stresses that the issue is still worrisome. At any given time, about one in 25 hospitalized patients has a health-care-associated infection while being treated for other conditions, leading to sepsis or death in many cases, according to the report.
“The Epicenter research by Washington University and BJC HealthCare is contributing to care improvements that protect the most vulnerable hospital patients from infections and other problems,” said John Jernigan, MD, director of the CDC’s Office of Prevention Research and Evaluation. “This dedicated team is literally saving lives.”
“The previous work of the WU-BJC Epicenter has dramatically lowered rates of catheter-associated bloodstream infections and ventilator-associated pneumonia in patients in intensive care units,” Jernigan said. “Given their successful track record, I can’t wait to see where the next phase of research takes us.”
Along with Harvard University, Washington University has participated in the CDC’s Epicenters Program since its inception in 1997. Other medical centers involved include the University of Pennsylvania, Duke University, the University of North Carolina, and the Chicago Prevention and Intervention Epicenter at Rush University Medical Center and Cook County Health and Hospitals System.
As part of the new funding, the School of Medicine is expected to participate in more than a dozen research studies, some in collaboration with other U.S. medical centers. The core projects for Washington University and BJC HealthCare include:
- Antibiotic use: Researchers will analyze antibiotic prescriptions in dental care throughout the U.S. in partnership with Express Scripts, the St. Louis-based pharmacy benefits manager. They will evaluate the extent and appropriateness of antibiotic use among dental patients and develop interventions to improve prescribing practices and promote antimicrobial stewardship programs among dentists.
- Infections following colorectal surgery: Researchers will examine the risk of surgical-site infections (SSIs) among patients undergoing colon surgery and implement interventions to reduce the risk of SSIs in diverse hospital and surgical settings.
- Infections among women undergoing mastectomies: Researchers will develop ways to assess the individual risk of post-surgery infections in breast cancer patients. They will take into account factors such as body mass index, diabetes, smoking, cancer stage, and type of surgical procedure, and will aim to tailor care regimens and treatments to prevent infections.
- Effects of fecal microbiome transplants on recurrent infections: Researchers will analyze the effects of fecal microbiome transplants administered to patients with recurrent Clostridium difficile. They suspect that transplants with healthy intestinal microbiota prevent C. difficile recurrence and decrease the development of multidrug-resistant bacteria from colonizing the intestinal tract.
- Identify biomarkers for urinary tract infections (UTIs): Researchers will analyze biomarkers and metabolomics profiles to develop new methods to improve UTI diagnosis and target more appropriate antibiotic use. UTIs are common and often caused by multidrug-resistant organisms. However, confirming a diagnosis can take several days. Current treatment practices often entail prescribing antibiotics even before a diagnosis is confirmed, which sets the stage for antibiotic overuse. New rapid UTI diagnostic tools can improve antibiotic use and reduce antibiotic resistance.
“The results of our research can significantly and positively impact public health because the findings can be quickly translated into improved clinical diagnostic tools, guidelines and practices in diverse health-care settings,” Fraser said. “Ultimately, this will reduce morbidity, mortality and costs from infections in health-care settings as well as antimicrobial resistance.”
The School of Medicine’s co-investigators include Hilary M. Babcock, MD; Carey-Ann D. Burnham, PhD; Gautam Dantas, PhD; Erik R. Dubberke, MD; Michael J. Durkin, MD; Jeffrey P. Henderson, MD, PhD; Kevin Hsueh, MD; Jennie H. Kwon, DO; Margaret A. Olsen, PhD; and David K. Warren, MD.







