Using data to improve kidney transplant outcomes, personalize care
Analyzing national kidney transplant databases could help improve patient care and outcomes
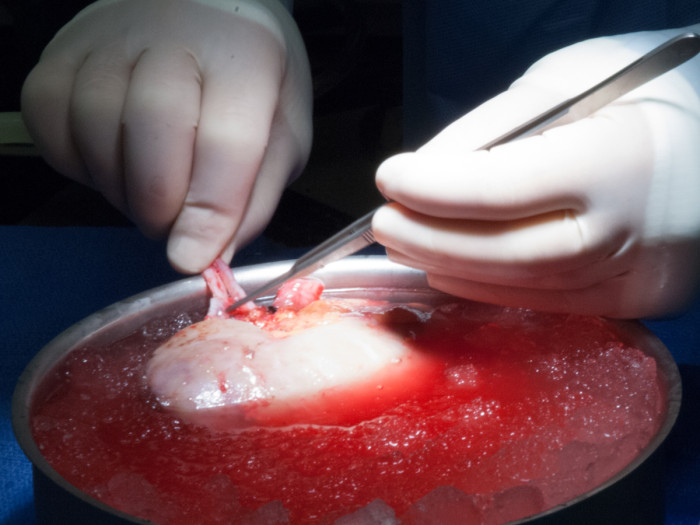
Determining the proper care after a kidney transplant is often a delicate balancing act. One key aspect involves choosing the right combination of medications to avoid organ rejection and minimize potentially crippling complications.
“Many transplant drug regimens change over time for patients,” says Vikas Dharnidharka, MD, director of the Division of Pediatric Nephrology in the Department of Pediatrics at Washington University School of Medicine. “In some ways, it’s an art to determine which medications should be given at which time.”
Analyzing data about transplant medications and complications can help with this process. But it is difficult to amass enough data from any one center, which may only perform a few hundred kidney transplants a year. So researchers like Dharnidharka rely on data from national databases, which have historically been difficult to interpret.
He and his colleagues hope to change that.
The researchers are working with a combination of national databases to analyze and track complications related to transplant, patient progress over time and other key data points with the goal of improving patient care and outcomes.
Mining massive datasets
Federal law requires that all certified transplant centers enter patient information into a national transplant database. The data that care providers enter into this database include:
- Information about the transplanted organ
- Transplant success rates
- Prescriptions written at the time of transplant
- Other information related to the transplant
By further linking to and analyzing national pharmacy databases, the researchers can also determine medications patients receive after their initial recovery and over prolonged time periods. Unfortunately, the national transplant database does not list all patient complications. This is why the team also consults and links to an insurance database, which contains claims submitted when treating infections or other complications patients may have developed over time.
The team makes sure to access the data in a manner that complies with national confidentiality and health compliance policies. To further ensure they meet all privacy standards, the researchers store all data in one highly secure location that cannot be accessed remotely.
By cross-referencing these massive datasets, the team has found that approximately one quarter of patients had an episode of pneumonia during hospitalization within the first year after their kidney transplant. The researchers also discovered that about 20 percent of patients developed sepsis, a severe inflammatory reaction to infection. The risk for these complications is different based on a patient’s underlying characteristics and what medicines they initially started on after transplant.
“We knew these sorts of complications occurred in transplant patients, and that they are not trivial. But trials have not traditionally reported these sorts of data well.” This is where the combined database information has been key, says Dharnidharka.
Predicting complications
By combining and automating analyses of these disparate datasets, Dharnidharka and his colleagues are developing a free web-based tool that they hope will be able to determine patients’ likelihood of developing complications after transplant. Using a patient’s age, gender, initial diagnosis, family history and other data, their goal is to determine a patient’s risk for major complications.
“Now we have gathered data that should be able to show your three-year risk for complications such as pneumonia or sepsis based on the regimen you started with,” says Dharnidharka.
Currently, transplant centers have standard regimens that all patients receive, similar to a “one-size-fits-all” approach. But by analyzing each patient’s data separately, Dharnidarka and his colleagues would like to individualize this care. His team is the first to attempt to evaluate this massive amount of information in such a strategic manner. “We hope this tool will be able to give the physician and the patient an overview that allows them to make more personalized decisions.”