Scientists more effectively control pain by targeting nerve cell’s interior
Blocking receptors stems chronic pain, suggests options for pain relief with fewer side effects
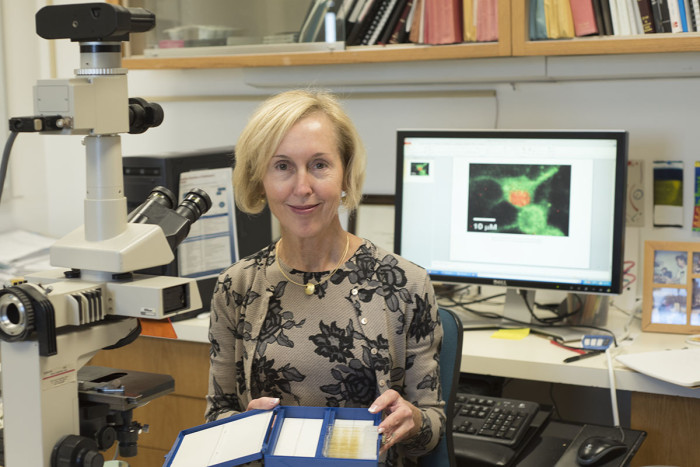 Robert Boston
Robert BostonKaren O'Malley, PhD, led a team that discovered that in nerve cells, the location of receptors that transmit pain signals is important in how big or small a pain signal will be. O'Malley's computer screen shows receptors (orange) in the nucleus of a nerve cell that have been activated by a drug that targeted those nuclear receptors rather than receptors on the cell surface.

In real estate, location is key. It now seems the same concept holds true when it comes to stopping pain.
New research at Washington University School of Medicine in St. Louis and McGill University in Montreal indicates that the location of receptors that transmit pain signals is important in how big or small a pain signal will be and how effectively drugs can block those signals.
Blocking pain receptors in the nucleus of spinal nerve cells could control pain more effectively than interfering with the same type of receptors located on cell surfaces, the research shows. The scientists also found that when those same nerve cells encounter a painful stimulus, some of the receptors migrate from the cell surface into the nucleus.
“Chronic pain affects almost 30 percent of Americans, and we’ve found, in rats, that by blocking specific receptors inside the cell, we can block pain,” said co-senior author Karen O’Malley, PhD, a professor of neuroscience at Washington University. “If we can find ways to specifically block pain receptors inside of cells rather than on the cell surface, we may make a big dent in chronic pain with fewer drug-induced side effects.”
The study is published online Feb. 3 in the journal Nature Communications.
The researchers focused on a specific type of glutamate receptor that is part of the family of receptors called G-protein-coupled receptors, which are important in signaling between neurons.
In a rat model that mimics a type of chronic, neuropathic pain, animals treated with investigational drugs to block the activity of the receptors in the nucleus responded in ways suggesting they had gotten relief from their pain.
“Drugs that penetrate the spinal nerve cells to block receptors at the nucleus were effective at relieving neuropathic pain, but those that didn’t penetrate the cells were not,” said McGill’s Terence J. Coderre, PhD, who developed the rat model.
Coderre also explained that rats with nerve injuries displayed less spontaneous pain and less hypersensitivity to a painful stimulus when those nuclear receptors were blocked. But normal rats without nerve injuries had no changes in pain sensitivity when those receptors were blocked and the animals were exposed to a painful stimulus.
“This is the first time we’ve been able to demonstrate that receptors inside the cell, on the nucleus, affect behavior in living animals,” O’Malley said.
Coderre quipped: “By engineering drugs to target glutamate receptors at the nucleus, I guess you could say that pain treatment has gone nuclear.”
Scientists have been studying glutamate receptors in the pain pathway for decades. What’s new, O’Malley explained, is that these most recent experiments — in cell cultures and rats — demonstrate that the location of the receptor in the cell has a major effect on the cell’s ability to transmit pain signals.
For example, the researchers found that when these particular glutamate receptors on the nucleus of a nerve cell were activated, the response — measured by the amount of calcium released— was nine times larger than when the same type of receptor was activated on the cell’s surface. Changes in calcium levels play a key role in signaling in neurons. Increased calcium can release important neurotransmitters, regulate specific genes and contribute to synaptic changes that are critical to pain signals.
“The nuclear calcium response goes up and stays up for a significant period of time — about four minutes,” O’Malley said. “The increased levels of nuclear calcium activate pathways that carry pain signals from the nerves to the brain.”
They also found that the glutamate receptors on the nucleus responded to painful stimuli more robustly than the same types of receptors located on the cell’s surface, and that when the cells encountered such a stimulus, some receptors migrated from the surface to the nucleus. The researchers also discovered that receptors located in the nucleus stopped activating pain signals when targeted with drugs.
The researchers focused mainly on nerve cells in the spinal cord, an important area for transmitting pain signals coming from all parts of the body. Future research will be aimed at determining what events cause the glutamate receptors to migrate to the nucleus and how to make drugs that more specifically block only glutamate receptors in the nucleus of the nerve cells.