Potential drug target identified for deadly brain cancer
Researchers identify key protein in brain tumor formation
 Albert Kim
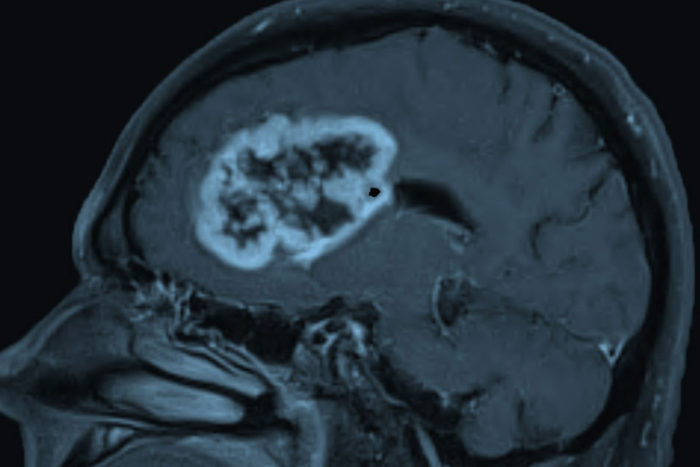
Albert KimGlioblastoma, shown above, is the most common and deadly form of brain cancer in adults. New research at Washington University School of Medicine in St. Louis shows that glioblastoma patients with a protein called oncostatin M receptor on their tumors face a particularly poor prognosis, suggesting that treatments that target the protein could improve survival.
Glioblastoma is the most common and deadly form of brain cancer in adults, with an average survival time of only 15 months after diagnosis. New research at Washington University School of Medicine in St. Louis provides clues to why some patients with glioblastoma fare worse and identifies a drug target that potentially could improve survival.
The research shows that glioblastoma patients with a protein called oncostatin M receptor on their tumors face a particularly poor prognosis. Further, the findings suggest that treatments that target the receptor have the potential to halt progression of the especially aggressive tumor.
The research is available online in Nature Neuroscience.

“None of the treatments developed for glioblastoma over the past decades has been effective,” said senior co-corresponding author Azad Bonni, MD, PhD, the Edison Professor of Neuroscience and head of the Department of Neuroscience at Washington University. “We wanted to go back to the basic science and understand how these tumors arise so that we can identify new targets for potential therapy.”
Tumors arise when cells accumulate mutations that allow them to escape normal constraints and start multiplying uncontrollably. The typical tumor cell carries mutations in multiple genes, and the effect of mutating one gene can depend on which other genes also are mutated in the cell.
For example, earlier work by Bonni and colleagues at Harvard Medical School had shown that a protein called STAT3 protects against tumor formation, unless a mutated form of another protein, epidermal growth factor receptor (EGFR), is present. In such cases, STAT3 switches from protecting against tumor growth to actively promoting tumors.
More than half of glioblastoma tumors contain mutations in the gene for EGFR or the sections of DNA that control how much EGFR is produced. Researchers reasoned that since mutated EGFR promotes tumor formation, inhibiting it should shrink tumors. Drugs that target EGFR, however, have had little effect on the survival of glioblastoma patients.
“It looked like we were missing something in the EGFR-STAT3 pathway,” Bonni said. “If inhibiting EGFR didn’t work, maybe it was because we needed to hit something else, too.”
Using brain tumor stem cells derived from human tumors, Arezu Jahani-Asl, PhD – lead author of the study and an assistant professor at McGill University – and colleagues looked for other genes in the pathway. They found that the oncostatin M receptor, a protein associated with cell proliferation, was produced in cells that carried both STAT3 and the mutated form of EGFR. Furthermore, the receptor paired up with the mutated EGFR to trigger the production of even more of the receptor in a positive feedback loop.
“Oncostatin M receptor started looking like an important target because it amplifies the EGFR pathway, which we already know is important in glioblastoma,” Bonni said. “But before going further, we asked, ‘Is this really relevant to human patients?’”
Two publicly available databases collect information about the molecules expressed on tumors from individual patients and how long those patients survived. In both datasets, the researchers found that the more oncostatin M receptor on the tumor, the sooner the patient died.
The researchers then removed the receptor gene from human brain tumor stem cells and injected the modified cells into mice. The cells lacking the receptor formed tumors a fraction of the size of those formed by the same human brain tumor stem cell line with the receptor, indicating that the protein plays a key role in tumor formation, growth or both.
“Being able to stop tumor formation entirely was a dramatic and shocking result,” said senior co-corresponding author Michael Rudnicki, PhD, a professor at the University of Ottawa. “It means that this protein is a key piece of the puzzle and could be a possible target for future treatments.”
Scientists now are looking for drugs that can inhibit the receptor or block its interaction with EGFR. Such drugs potentially could lengthen survival times for glioblastoma patients.
“It really gets down to personalized medicine,” Bonni said. “People whose tumors don’t express the receptor wouldn’t see an effect. But for people who overexpress the receptor, blocking it might really help.”